Overview:
- Summary of All Notes Here: Matt Walker TED Talk on Sleep
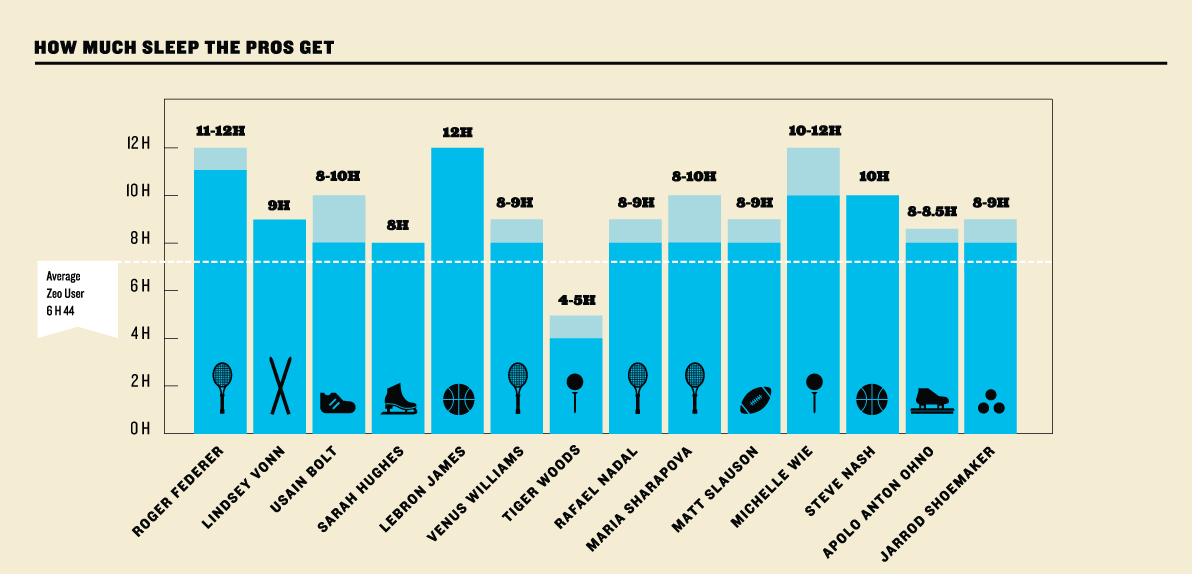
- Great sleep infograph statistics.
- There is no physiological system that we’ve been able to measure that isn’t wonderfully enhanced by sleep when you get it, or demonstrably impaired when you don’t get enough.
- If you’re lucky enough to have a lifestyle that allows you to go to bed within about two to three hours after sunset and then wake with the sunrise, that’s ideal. That’s the way that nature is supposed to operate. However, we live in a post-industrial era. I doubt any of you are going to be in bed about an hour from now. – BG
- Justification for prioritizing sleep: I don’t want to die young and I don’t want sickness and disease in my life.
- When you look at the evidence of decreasing almost every disease that is killing us in the developed world it’s very hard to look no further than the importance of sleep. – MW
- All of studies of telling us the shorter your sleep the shorter your life. – MW
- When we think about diet and movement/activity being key components of health alongside of sleep people like to play a head to head hierarchical game against them from imm1-3. But I don’t think we need to do that under the consideration that sleep is the foundation to which the other 2 pillars or diet and movement sit on. Or sleep is the foundation whictvh optimal health sits on. – MW
- You could make the case that going without sleep is one of the quickest if not the quickest way to decrease function and lead to death alongside of hydration. – MW
- The Guinness world record has actually banned the attempts of going without sleep that should highlight the imperative nature of sleep on survival.
- Timing your sleep with the synchrony of the natural light-dark cycle (sun rise/set) without an alarm seem’s to be the most natural effective way to regulate sleep around our modern world.
- Midnight: “Have you ever thought about what the term midnight actually means?” You know, it means the middle of the solar night, which is the time when most of us should be in the middle of our sleep phase.
- One out of every two adults in first world nations is chronically sleep-deprived.
- “There is truly no aspect of a human being’s wellness that isn’t eroded by a lack of sleep. Lack of sleep is like a broken water pipe in your home. . .it will leak down into every nook and cranny of your physiology.”
- “Ours is a culture where we wear our ability to get by on very little sleep as a kind of badge of honor that symbolizes work ethic, or toughness, or some other virtue… …but really, it’s a total profound failure of priorities and of self-respect.” – Maria Popova
- “10-15% of the protein-encoding human genome is regulated by the sleep-wake cycle. 40–50% of those genes deal with metabolism (Source)
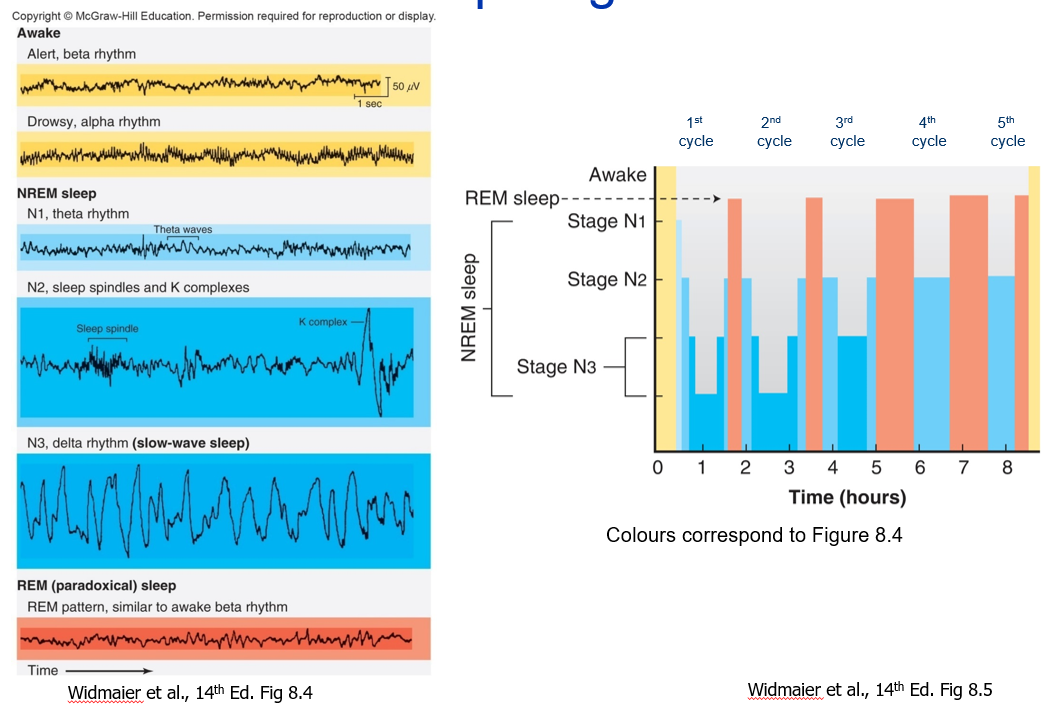
Stages of sleep, sleep cycles, and brainwaves
Humans (Mammals) have 2 stages: NREM & REM
- Awake/Alert: Beta Waves
- Brainwaves when first lie down: drowsy (before you fall asleep): Alpha Waves
- Back of brain (visual brain), stops processing the outside world, frequency slows from 50 cycles/sec slowed to 10 cycles/sec (still relatively low amplitude)
- Transitioning to sleep: Eyeballs start to roll (slow rolling eye movements) first sign of transition to sleep (reason is unknown)
- First you go into the light stages of non-REM stage 1 and 2
- After 20 minutes you are into the deep stages 3 and 4
- Stages of non-REM:
- Stage 0: Wake: Awake time is the time spent in bed before and after falling asleep. It also includes brief awakenings during the night. These episodes are completely normal for healthy adults.
- Stage 1: NREM: theta waves begin (lightest stages of sleep)
- Stage 2: NREM: Synchronous bursts of electrical activity called sleep spindles (a second and half long) and K complexes ⇒ Big slow wave, then burst of spindle (lightest stages of sleep)
- Light sleep initiaLight sleep initiates your sleep cycle and acts as a transition to deeper sleep stages. During this stage your muscles begin to relax, your heart rate and breathing slow down, and you wake up easily.tes your sleep cycle and acts as a transition to deeper sleep stages. During this stage your muscles begin to relax, your heart rate and breathing slow down, and you wake up easily.
- During light sleep, you can expect the following: muscles relax and may jerk respiration slows heart rate decreases body temperature drops sleep begins
- Stage 3 & 4: During this deep sleep, we get info transfer in brain (delta waves – slow wave sleep) – very deep restorative stages
- It is the most rejuvenating and restorative sleep stage, promoting muscle growth and repair as well as waste removal in your brain. In this stage, you have difficulty waking up and are disoriented or groggy if awoken.
- , you can expect the following: blood pressure drops blood flow increases to muscles repair hormones (i.e. growth hormone) are released tissue growth and cell repair occurs long, slow brain waves brain flushes out waste
- Stage R: REM sleep: (REM=Rapid eye movement, based on the bizarre horizontal shifting eye movements) Mix of theta/beta similar brain waves to wakefulness (paradoxical sleep)
- associated with dreaming, memory consolidation, learning, and problem solving. The time spent in this sleep stage usually decreases with age.
- increased heart rate; increased respiration; paradoxical sleep
- you can expect the following: respiration increases heart rate increases temperature regulation is switched off brain activity is high; vivid dreams may occur body becomes immobile to stop you from acting out dreams blood flow increases to genitals
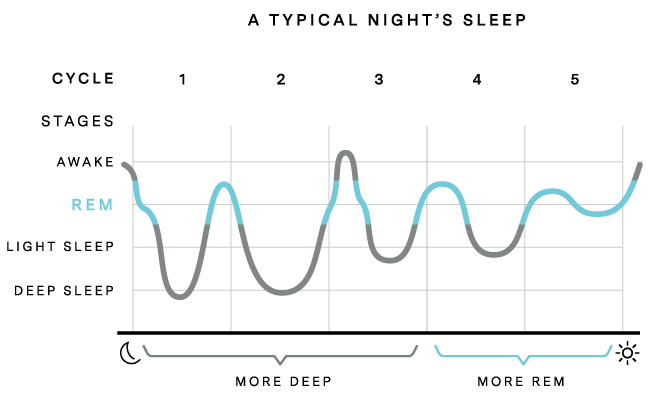
Your body cycles through these stages four to five times each night. Cycles earlier in the night tend to have more NREM sleep while later cycles have a higher proportion of REM. By the final cycle, your body may even skip NREM deep sleep entirely. Overall, your body spends more time in NREM phases of sleep.

Stages must occur in order with 2 exceptions:
- 1) Narcolepsy – from awake straight into REM
- 2) If chronically REM sleep derived, occasionally into REM sleep directly (e.g., heavy alcohol use)
Summary of the 90 minute cycle:
- Go through stage 1-4 on non-REM
- Then after 70 min, you go back to stage 2 on non-REM
- Then you will briefly transition to REM sleep
- Then you flip flop between non-REM and REM ⇒ back down into non-REM, back to REM, back to non-REM, back to REM
90min sleep cycles:
- Every 90 minutes, your brain cycles between non-REM and REM sleep
- Then this is replayed every 90 minutes to create what we call a standard cycling architecture of sleep, or what we call a hypnogram of sleep.
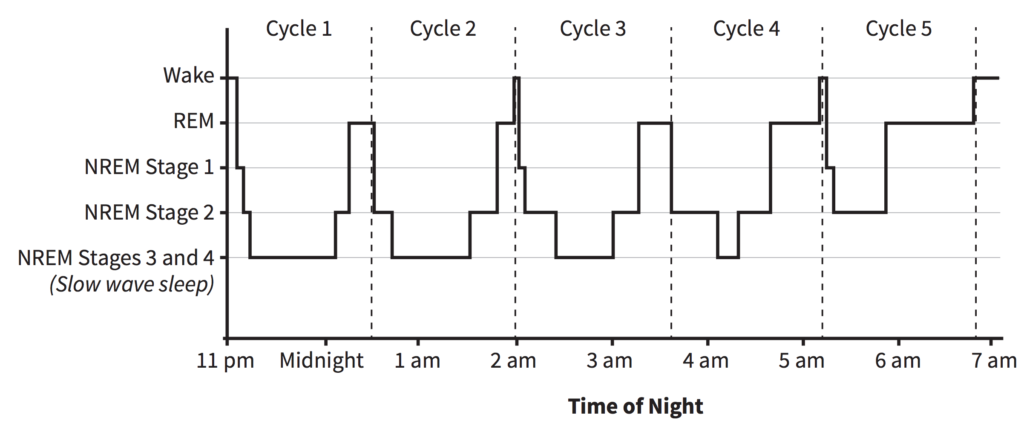
What changes is the ratio of non-REM to REM within that 90 minute period, as you move across the night:
- In first half of night, majority of 90 minute cycle is deep non-REM
- In the second half of the night, the majority of cycle is REM
- If get 6 hours sleep (instead of 8), you’re losing 25% of sleep, but could be losing up to 70% of all REM sleep
Implications:Disrupting Brain Activity During REM Sleep Can Stop The Brain From Remembering Things Learned That Day:
- “Disrupting the activity only during REM sleep, and not other sleep, basically obliterates consolidation and memory formation,” Dr Williams said. For example, if it was shown one brand new object and one that it had seen the day before, the mouse would thoroughly investigate both, instead of concentrating – like a normal mouse would – on the unfamiliar one. [Source]
Sleep Patterns:
- Increase in deep sleep after a hard workout: Exercise can increase your body’s prioritization of deep sleep the night after an intensive workout.
- Higher REM rebound after sleep deprivation: When you recover from a period of sleep deprivation, your body prioritizes deep sleep for the first few nights to repair your body and prepare for action. After several nights of sufficient deep sleep, REM sleep rebounds to focus on your brain (does that mean I’m not rebounding because I’m usually on the border of sufficient deep sleep?)
- Interrupted sleep cycles after caffeine: Caffeine can increase the time it takes for you to fall asleep, cutting your sleep period short. Shorter sleep periods disproportionately cut down on your total REM sleep, as REM cycles are more likely to occur in later sleep cycles.
The 4 Pillars of Sleep (RCQQ)
- Regularity (consistency of sleep schedule) e.g. are you feeling asleep at 1am then 10pm then 12am.
- Continuity (waking up many times per night?) e.g. is it fragmented, are you waking up multiple times or are you sleeping straight through?
- Quantity (in total, and in each stage) e.g. how much sleep are you getting and how much of each different stage of sleep.
- Quality (how good the “electrical signature” of sleep is; caffeine, alcohol, etc. can have an effect on quality) e.g. just because your getting 8h of sleep doesn’t mean your getting 8h of good electrical quality deep sleep.
⇒ Alzheimer’s is very complex: Different sleep features will be predictive of different aspects of the amyloid pathology cascade.
Lighting Resources:
- Lighting globe company Heal The Lighting SLEEPY BABY BULB (Ben Greenfield)
- Low-temperature Red incandescent bulbs
- What you can do is you can replace all the lightbulbs in your house with red, orange, yellow, or any form of blue light free bulbs.
- Bedtime Bulb Low-Blue Light Bulb for Healthy Sleep and Baby
- Now, if you’re going to have guests over and you’re concerned about their impression, or your family isn’t going be cool with colored lightbulbs: Vintage Incandescent Edison Light Bulbs: 60 Watt, 2100K mWarm White Lightbulbs – E26 Base – Dimmable Antique Filament Light Bulb
- the ones that you’ve seen in restaurants also that have the filament exposed. They’re very beautiful, but make sure you get the incandescent ones. You can get them on Amazon, too, not the knockoff ones with LEDs that are made to look like the incandescent because those are way stronger, more blue light, and not good.
- So, what these Thomas Edison bulbs are good for is that they’re much dimmer than most other lightbulbs available, which is great at night, and they have very little blue light, but they still look pretty normal, natural, and they’re beautiful.
- Candles with wax that doesnt emit toxic chemicals
Chronotype: Propensity to Sleep at a Particular Time
Chronotype Quiz: https://thepowerofwhenquiz.com/
- your chronotype simply determines whether you’re a morning person, an evening person, or somewhere in the middle, about 30% of the population is an extreme morning type or a morning type (larks)
- about sort of 40% percent is sort of neither strongly morning or evening, and about the remaining
- 30% is an evening type, we call them (owls)
- Many owls think that they have insomnia. They don’t. They’re just not going to bed at the right time.
- So if you’re a morning type, you like to go to bed, let’s say, like, 9 p.m. And wake up at 5 or 6. If you’re an evening type, you may want to go to bed at 1 a.m. And wake up at 9 a.m. The next morning.
- So when I’m saying the optimal position of sleep, I’m saying with the optimal for your chronotype.
- And by the way, it’s genetic. You don’t get to decide whether you’re a morning type or an evening type. It’s hardwired into your genes. We know the genes. It’s not your fault. If you’re an evening type and you’re listening to this, and society, which is strongly architected against your chronotype, we reward and we favor the morning types, it is not your fault. It’s not a choice. And there’s not too much you can do about it. You can push and pull the system by about 30 minutes, 45 minutes, but not much more.
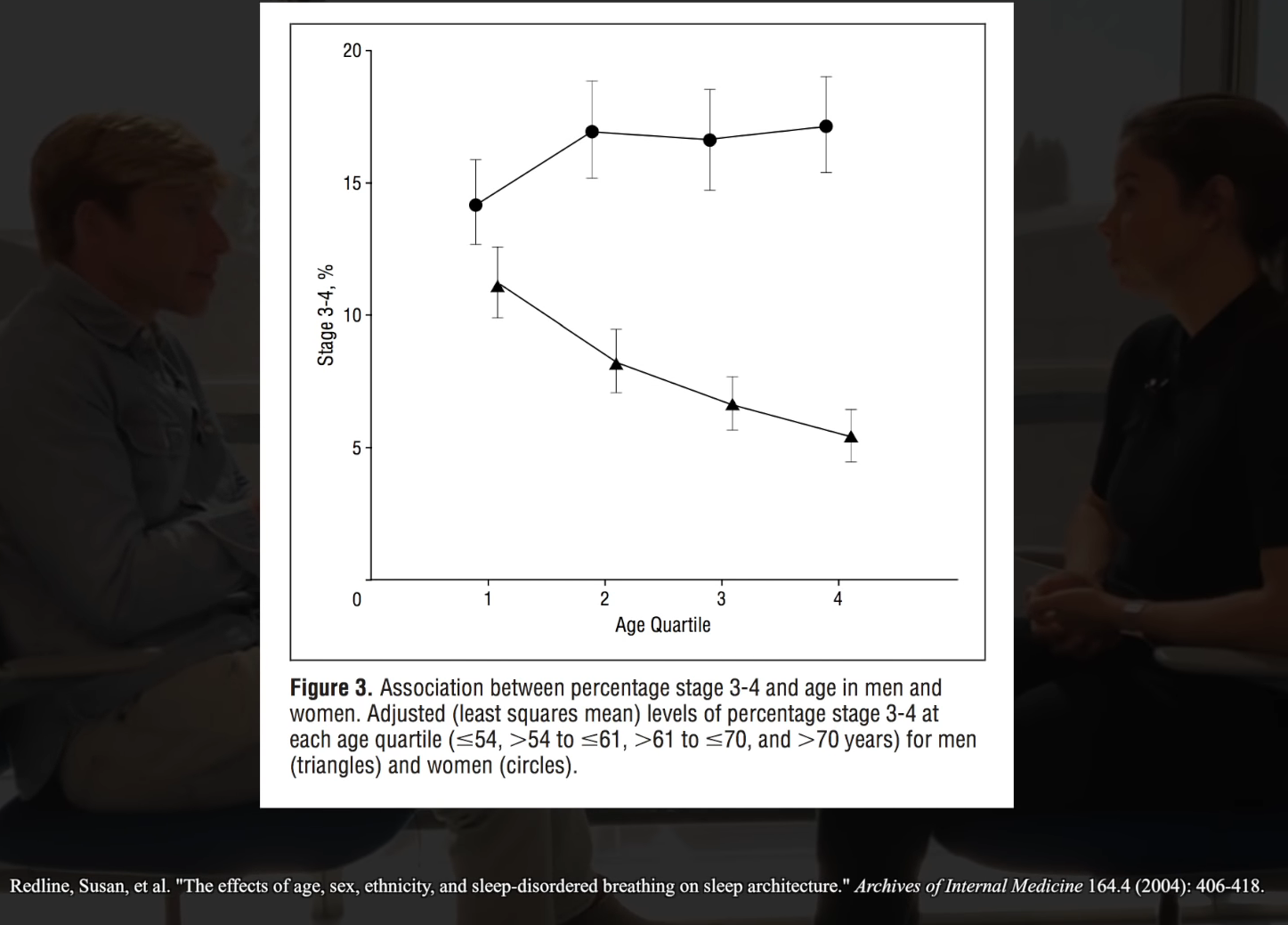
Age & Deep Sleep Reduction
- We can see the decline of deep sleep occurring in people in their 20s. That’s when your deep sleep starts to decline.
- By the time you’re 50 years old, you’ve lost about 50% of the deep sleep that you are having when you are a young teenager. By the time you’re 70%, there’s only about about 5% of your deep sleep left that you had when you were young and healthy. By the time you’re 80, we almost can’t detect any of these deep sleep brain waves anymore.
Sleep & Alzheimer’s Disease
Could sleep disruption be a bio-marker of dementia, or even an underlying cause?
- “Based on the weight of the data that we have, the evidence, I think it is causal. I think that sleep, at this stage, may be one of the most significant lifestyle factors that determines your risk ratio for Alzheimer’s disease. I feel the causal evidence for that now in humans and animals is strong enough to make that statement. And I don’t make that statement lightly.” – MW
- The first thing is that we see that within insufficient sleep, you get increases in oxidative stress pathways and that leads to a whole cascade of things that lead to neuronal death. One of the areas in the brain that is most sensitive to this is the hippocampus which is a critical memory center. – MW
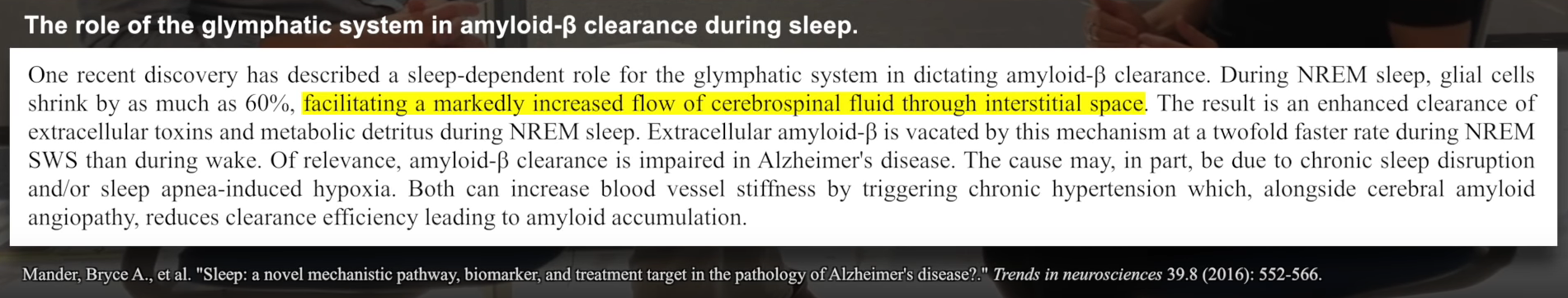
The Glymphatic System (GS): What Happens During Deep Sleep
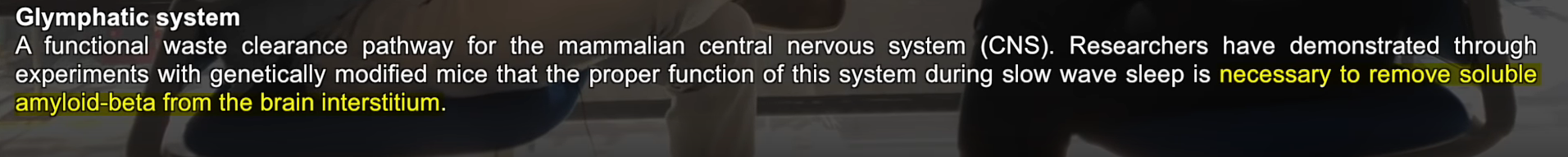
- The glymphatic system is activated 10-20 folds during deep sleep. During these slow brain wave stages the brain squirts cerebral spinal fluid into the brain in between extracellular space (in between neurons) and basically clears out dead cellular debris, protein aggregates, amyloid beta-plaques – its literally like a cleaning system that squirts and washes everything out of the brain.
- Side Note: Some studies have shown intense exercise can improve the length you stay within deep sleep.
- Remarkable discovery: In 2012, Rochester University team found that brain has “sewage” system called the glymphatic system (named after the cells in the brain that form the system called glial cells) similar to lymphatic system in the body.
- These glial cells forms this sanitation system that kicks in when in deep sleep and glial cells shrink up to 60% in size making room for cerebral spinal fluid fill brain to start perfusing the brian and washing out the “metabolic detritus” caused from wakefulness. – MW
Figure 1. Schematic depiction of the glymphatic pathway. In this brain-wide pathway, CSF enters the brain along para-arterial routes, whereas ISF is cleared from the brain along paravenous routes. Convective bulk ISF flow between these influx and clearance routes is facilitated by AQP4-dependent astroglial water flux and drives the clearance of interstitial solutes and fluid from the brain parenchyma. From here, solutes and fluid may be dispersed into the subarachnoid CSF, enter the bloodstream across the postcapillary vasculature, or follow the walls of the draining veins to reach the cervical lymphatics. Image credit:(Iliff et al., 2012)
How is this related to Alzheimers Dementia (AD)?
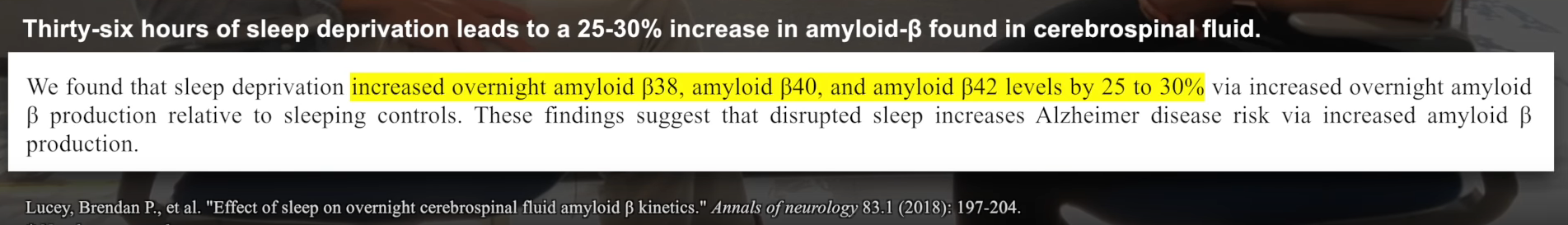
- β-amyloid is one of things washed away by the GS, a core toxic protein in Alzheimer’s formation which escalates Alzheimer’s risk.
- Therefore if you’re not getting quality amount of sleep your not getting that washing away of β-amyloid so your building more β-amyloid as sleep deprivation continues. Doing that night after night is like compounding interest on a loan escalating your Alzheimers risk.
- PET scans were done on groups people in their later elderly life according to sleep reported across a lifespan to map the amount of β-amyloid in the brain:
- Though this is only associational data from an epidemiological study which has it’s many limitations.
- There were obvious differences with people getting 7 hrs of sleep or less, there is marked difference in amount of β-amyloid built up compared to 7 hrs or more. Again, this is just associational evidence, but when we analyse animal (rats) studies for further info, rates deprived of sleep or when their s leep is fragmented, get an immediate β-amyloid buildup in the brain.
- Study in humans: Take deep sleep away from a human for one single night and you can see significant increase in circulating levels of amyloid and tau the next day.
- They still got 8 hours total, but the way they took away their deep NREM sleep by playing auditory tones.
- As a result their GS “sewage system” never kicks into gear to clear those proteins out so toxic proteins like amyloid and tau build up.
- They do a spinal cord puncture and suck out some CSP and measure the 2 toxic proteins linked to Alzheimers amyloid and tau.
- The next day they saw after 1 night of sleep disruption a significant increase in circulating levels of amyloid and tau.
- At this point MW felt very comfortable purporting that sleep is a critical component for the prevention of Alzheimers disease.
- Side Q: Can street noise do that and have that low frequency effect that low frequency auditory tones played? We don’t know that yet. That’s a little terrifying if it can.
The role of β-amyloid in AD
- Amyloid-beta is a toxic 42-amino acid peptide that aggregates and forms plaques in the brain with age. Insufficient sleep increases the production of amyloid-beta. In turn, amyloid-beta deposition impairs sleep in a vicious, self-perpetuating loop.
- Peter Attia suspects β-amyloid may not main causal driver, more a result of AD. But if sleep is more about clearance than generation of β-amyloid, it is congruent with idea that other things on back end are driving it primarily
- Alzheimer’s so complicated because genetic predisposition + multiple pathways driving injury to very sensitive organ (brain) so sleep is not the only contributing factor clearly.
Tau and AD:
- Tau is a microtubule-bound protein found in the brain that forms the neurofibrillary “tau tangles” associated with Alzheimer’s disease. Tau tangles disrupt the transport of metabolites, lipids, and mitochondria across neuronal synapses where neurotransmission occurs. Diminished slow-wave sleep is associated with higher levels of tau in the brain. Elevated tau is a sign of Alzheimer’s disease and has been linked to cognitive decline.
- The data for Tau predicting AD and cognitive decline seems to be stronger than β-amyloid.
- Tau accumulation can also result from sleep insufficiency.
Why Are β-amyloid & Sleep Linked?
- The principal epicenter that generates your deep sleep sits right there in the middle part of the prefrontal cortex. It is exactly the same part of the brain that accumulates toxic beta amyloid protein.
- Long-term poor sleep predicts amyloid-beta deposition in the brain.
- Participants who had less slow wave sleep and poor sleep efficiency were more likely to have faster accumulation of amyloid-beta.
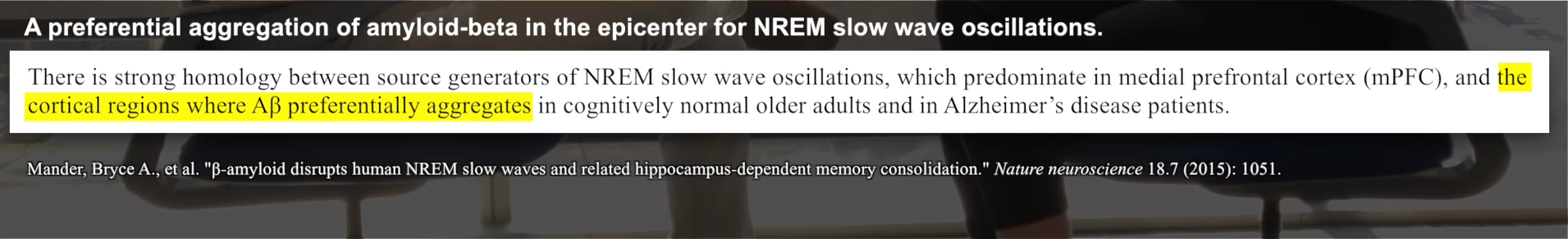
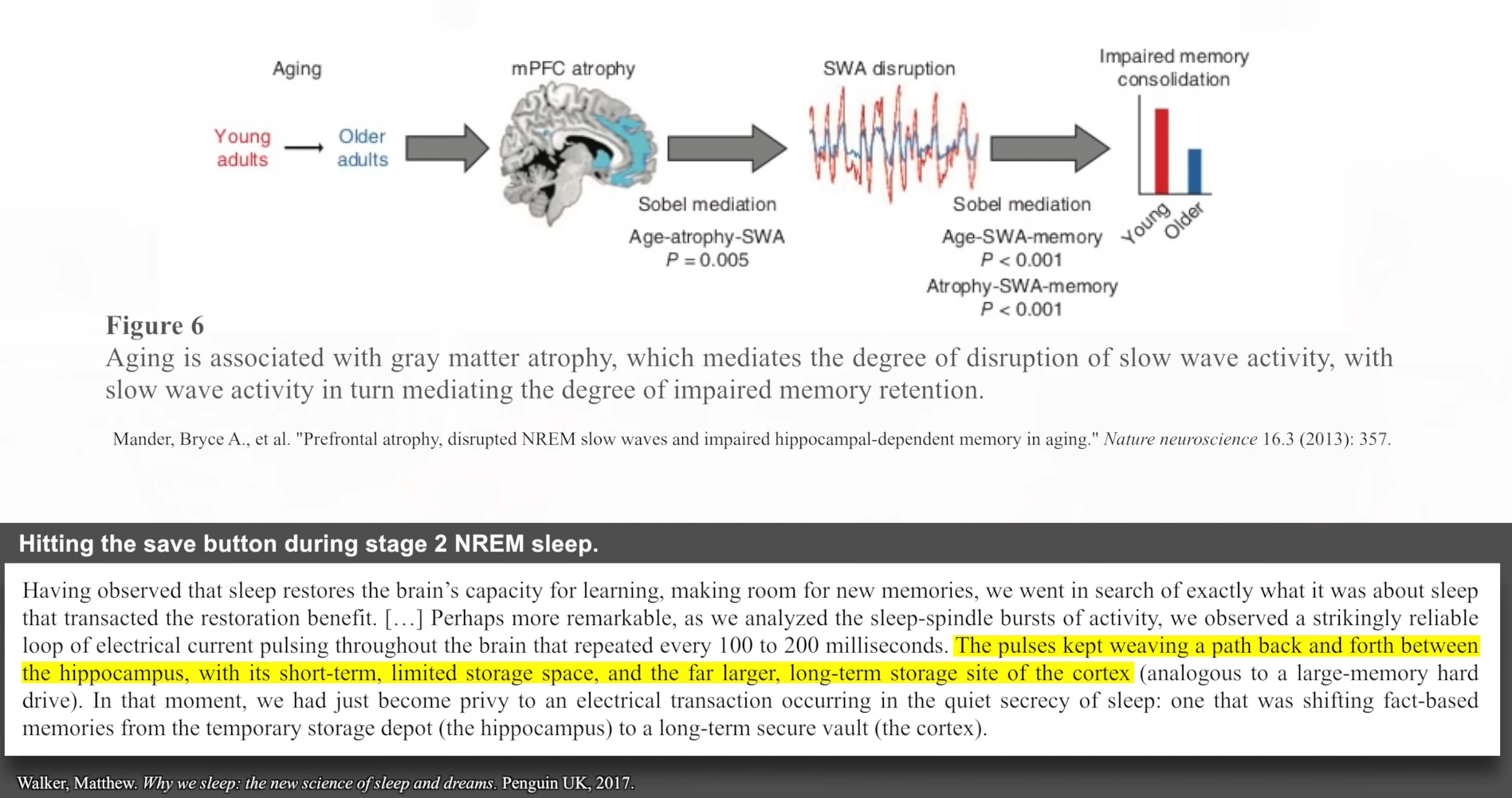
The more beta amyloid that builds up in this central frontal part of the brain, the less the deep sleep that you have. The less amyloid-related deep sleep that you had, the more forgetful you were the next day rather than the more that you remembered. So this was the first part of the Alzheimer’s sleep equation, which is that Alzheimer’s disease attacks the deep-sleep-generating regions and you have a decrease of deep sleep, which, in turn, blunts your learning and memory abilities and you become more forgetful.
Summary: If you’re not getting Enough deep sleep at night, you’re not giving yourself the chance for the kind of good night and sleep clean process to remove the beta amyloid. So more beta amyloid builds up. Where does it build up? Tragically, in the very same regions of the brain that generate the deep sleep that you need to clear out the toxic amyloid. So you start getting less deep sleep, so you get more toxic protein, more toxic protein, less deep sleep, less deep sleep. It’s a self-fulfilling prophecy, and it’s a nonlinear exponential curve.
Hormones & Sleep:
Sleep is balance among adenosine, cortisol, and melatonin (like an orchestra): Crescendo of adenosine – Then decrescendo of cortisol – Then melatonin comes in
Melatonin:
- Is a hormone produced in the pineal gland that plays a role in regulating sleep-wake cycles and sleep timing AKA when the brain is told to initiate sleep not so much to regulate the content of sleep. If our circadian conditions are optimal (meaning we’re not exposing our body to bright blue light before bed) we start to naturally produce melatonin 2-3h before sleeping.
- As we get older the meltonin we secrete over the night decreases which is where supplementation can be more efficacious.
- Dosage: More is not better with melatonin. 0.5mg~ appears to be the most effective in research. – MW
How Light Inhibits Melatonin Secretion #Post
- Melatonin secretion is controlled by the suprachiasmatic nucleus (SCN) of the hypothalamus, master pacemaker of circadian rhythms > Receive input from melanopsin found in the retinal ganglion cells (retina) > light detection sends AP to SCN suppressing melatonin secretion when light is detected’
Light & Food Being Signals for the Circadien Rhythm
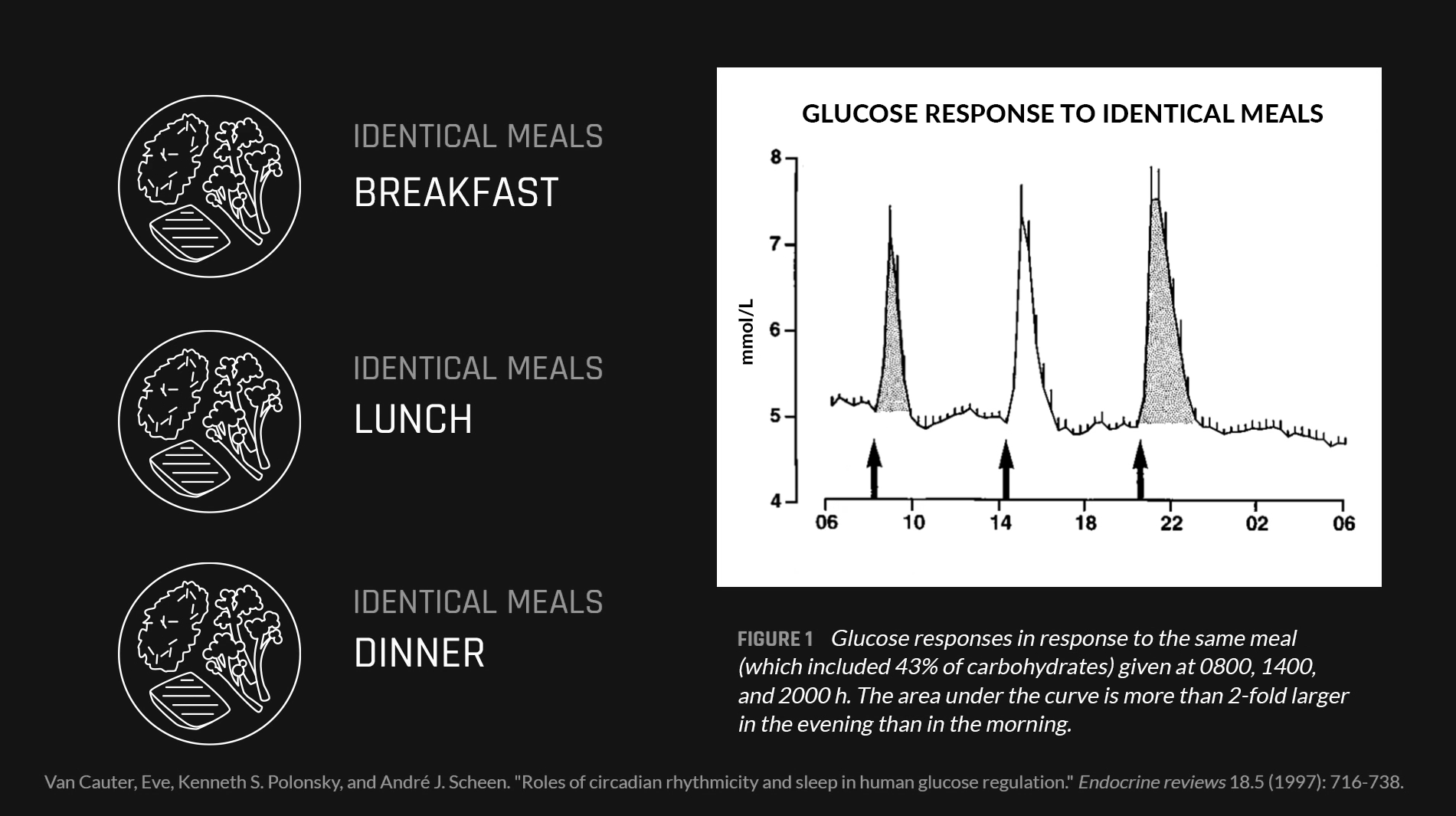
- What makes humans diurnal creatures is the presence of an internal clock in the brain referred to as the suprachiasmatic nucleus, or SCN for short. The part of this internal clock that interacts with the external cue of light, the SCN, is also referred to as the master oscillator. But light isn’t actually the only external cue we have, we also have food influencing what are known as peripheral oscillators that occur in peripheral tissues such as the liver and influence metabolism. Whereas light is the major cue for circadian rhythm, timing of food intake regulates circadian rhythm in peripheral tissues as well. This fact sort of helps to explain why time-restricted eating as it’s defined by Dr. Panda’s work and that of others begins with the eating period with the very first bite or drink of ANYTHING non-water, because even compounds that exist in black coffee such as caffeine, can be reasonably expected to produce metabolic effects that influence these peripheral oscillators, including activity in the liver.
- Everything from making neurotransmitters, to insulin, to glucose transport inside of cells, to oxidizing fatty acids, to repairing damage is on a 24-hour cycle clock that is influenced by these external cues involving metabolism.
When You Eat Matters
Circadian rhythms, the body’s 24-hour cycles of biological, hormonal, and behavioral patterns, modulate a wide array of physiological processes, including the body’s production of hormones that regulate hunger, metabolism, sleep, and others
- The impact of late night meals goes way back to our cave-dwelling roots. Before modern times, humans hunted and ate during the day and rested at night. Over time, our bodies developed networks of internal clocks, including ones in our digestive system (i.e., stomach, liver, and pancreas) to help us stay alert at biologically advantageous times.
- If you chow down on a late-night hamburger or brownie, it confuses your internal clocks. The one in your brain sees that the sun has set and is primed for sleep. However, the clocks in your digestive system kick into high gear, actively digesting at the very moment your other clocks are preparing for bed.
- You’ve now forced your body to sleep and digest at the same time—activities that the body has not evolved to do well simultaneously. This splits your body’s attention between two tasks, and it struggles to do a great job at either one. If your digestive clocks are synced up with your bedtime, sleep occurs more naturally.
Relationship between Food Intake and Sleep Pattern in Healthy IndividualsRESULTS:No differences in sleep patterns were observed in either gender, except in the percentage of stage 1 sleep, which was greater in men. Different correlations were observed between sleep and dietary variables according to gender. The correlation between dietary and sleep variables in men indicated a negative relationship between nocturnal fat intake and the sleep latency, including REM sleep. The percentage of nocturnal fat intake correlated with sleep efficiency, sleep latency, REM latency, stage 2 sleep, REM sleep, and wake after sleep onset (WASO) in women. The percentage of nocturnal caloric intake correlated with sleep latency and efficiency in women.
- Meal timing, and dinner timing specifically, may play a crucial role in determining sleep quality for the night ahead.
- Also, nocturnal rise in leptin and nocturnal levels of melatonin could be decreased because of late-night eating, although more evidence is required for this claim to hold.
Behavioral and Neuroendocrine Characteristics of the Night-Eating Syndrome
- In the behavioral study, compared with control subjects, night eaters had more eating episodes in the 24 hours (mean [SD], 9.3 [0.6] vs 4.2 [0.2]; P<.001) and consumed significantly more of their daily energy intake at night than did control subjects (56% vs 15%; P<.001). They averaged 3.6 (0.9) awakenings per night compared with 0.3 (0.3) by controls (P<.001). In night eaters, 52% of these awakenings were associated with food intake, with a mean intake per ingestion of 1134 (1197) kJ. None of the controls ate during their awakenings. In the neuroendocrine study, compared with control subjects, night eaters had attenuation of the nocturnal rise in plasma melatonin and leptin levels (P<.001 for both) and higher circadian levels of plasma cortisol (P = .001).
- During the daytime hours, the cumulative energy intake of the night eaters lagged behind that of the control subjects so that, in accordance with the selection criteria, at 6 PM they had consumed only 37% of their daily intake, compared with 74% consumed by the controls (P<.001). While the food intake of the controls slowed markedly by 8 PM, that of the night eaters continued at a rapid pace until after 12 AM. During the period from 8 PM to 6 AM, the night eaters consumed 56% of their energy intake, compared with 15% consumed by the control subjects (P<.001).
Why not eat 1-3h before bed? Because the TEF raises body temp. We know lowering body temp is really important to improve sleep quality and onset to sleep. So that’s why they say it. If you do eat late go for a walk in the cold and/or cold shower.
Eating Late Negatively Affects Sleep Pattern and Apnea Severity in Individuals With Sleep Apnea
- Late meal timing was associated with worse sleep pattern and quality and apnea severity than early meal timing. Despite some of these results having limited clinical significance, they can lead to a better understanding about how meal timing affects OSA and sleep parameters.
Melatonin Link to Insulin & Late Night Eating: Meal Timing *Post
- Melatonin has been shown to bind to receptors on the pancreas and this signals to the pancreas to stop producing insulin. That means our blood glucose levels will remain elevated because glucose is getting taken up into our cells. Practically speaking if someone is having a big meal when there is high melatonin release then there may not be enough insulin released from the pancreas and glucose may stay elevated for longer periods of time throughout the circulation.
- In 2009 a large genome wide assocation study was done (Prokopenko I, et al) and found people with diabetes or obesity might have a mutation in their melatonin receptor which was originally confusing because they originally thought ‘what does melatonin have to do with diabetes/obesity?’ 10 years later they looked at where the receptor was expressed and they found out this effect on melatonin on insulin.’
- Practically this means people who eat late into the night are likely to not get the best glucose control because their glucose might be elevated higher compared to if they had the same meal a few hours prior.
- Fatty acid metabolism is very similar andis tied to our circadian rhythm. We are generally less efficient at using fatty acids as energy in the evening compared to the during the morning.
- This is obviously very important for people with pre-diabetes or diabetes, but it’s also very important for gen pop who want to stave of these conditions and want to maintain brain function.
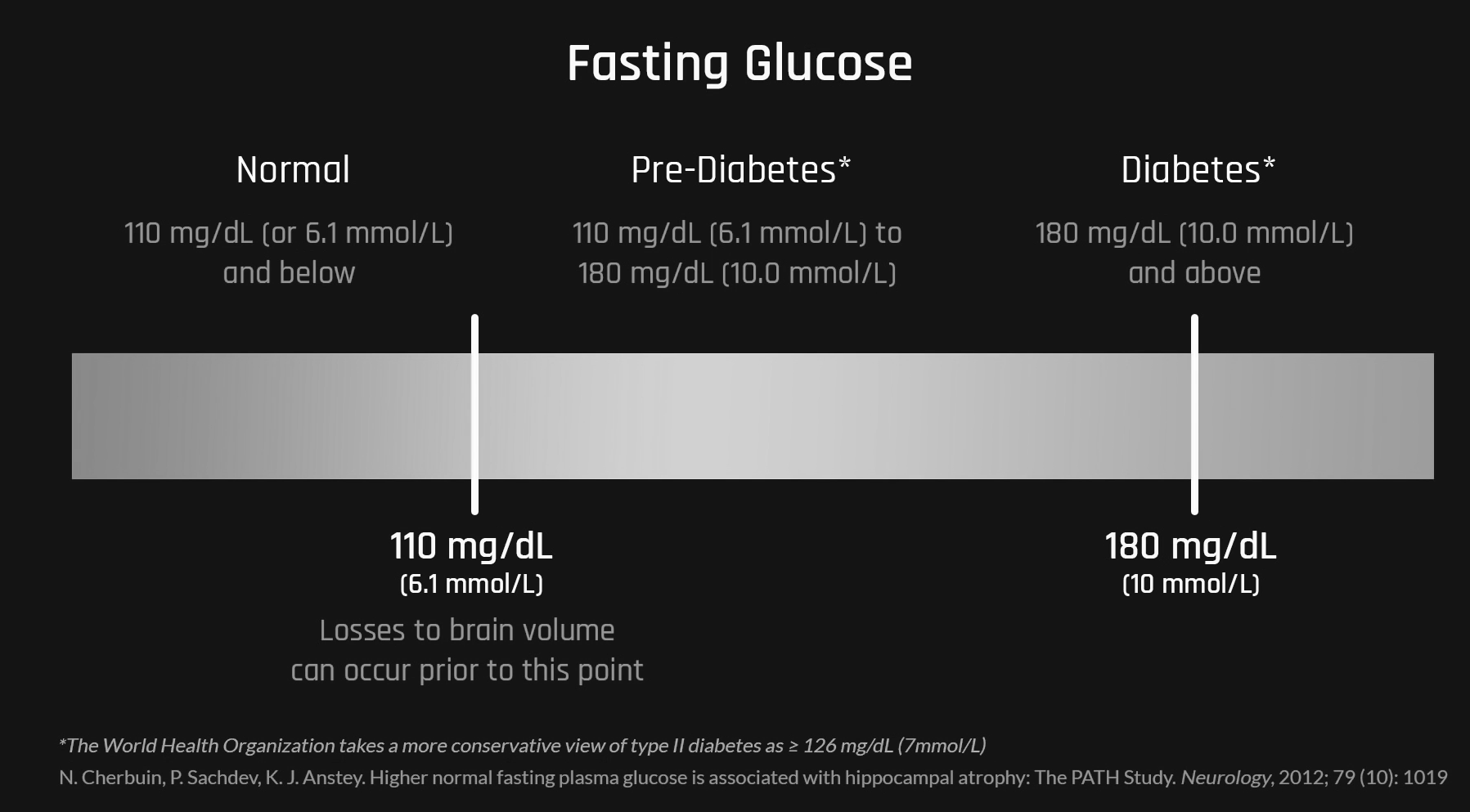
- One study found in an association of even high fasting plasma glucose levels within the ‘normal range’ (<100mgdL or <5.6 mmol/L) were associated with brain volume losses in the hippocampus and the amygdala, regions of the brain involved in memory, learning and cognition. These were ‘healthy people without diabetes’. “These findings suggest that even in the subclincal range and in the absence of diabetes monitoring and management of plasma glucose levels could have an impact on cerebral health.
- This drives home the importance of finishing off the last meal 2-3h before bed to better align with when our body is sending signals to shut down insulin production.
- 4 Young men had increased body fat in response to later meal timing independent of food content and activity level.
An Inverse Relationship Between Melatonin & Insulin Secretion: Last Meal 3H Before Sleep To Optimize Sleep/Melatonin Production
- you want three hours before bed after you finish your dinner. You don’t want to eat right up until bedtime because your insulin’s high, and again, that’s hurting your cognition. That’s again, giving you the same sort of insulin resistance problem, storing fat, you’re doing all the things that are not helpful.
- Since melatonin is secreted in a clearly diurnal fashion, it is safe to assume that it also has a diurnal impact on the blood-glucose-regulating function of the islet. This factor has hitherto been underestimated; the disruption of diurnal signaling within the islet may be one of the most important mechanisms leading to metabolic disturbances. The study of melatonin–insulin interactions in diabetic rat models has revealed an inverse relationship: an increase in melatonin levels leads to a down-regulation of insulin secretion and vice versa. Elucidation of the possible inverse interrelationship in man may open new avenues in the therapy of diabetes. [Source]
Eating earlier in the day promotes lipid oxidation (fat burning)
- A new study suggests that circadian rhythms influence body weight by impairing lipid oxidation – the burning of fat.
- Method: The small study, which was conducted in two sessions, involved six healthy adults between the ages of 51 and 63 years old whose BMIs were between 22.2 and 33.4 (normal to obese). During the first session, the participants received three meals per day: breakfast (700 calories), lunch (600 calories), and dinner (1,000 calories). The second session differed in that, instead of receiving breakfast, the participants received a late-night (10 PM) snack (700 calories). The overnight fast was approximately 14 hours, regardless of whether the participants ate breakfast or the late evening snack.
- Results: The authors of the study monitored the participants’ metabolism in a whole-room respiratory chamber during the two sessions, which lasted 56 hours each. They found that eating a late-night snack rather than an isocaloric breakfast markedly altered the participants’ capacity to burn fat, and this shift in metabolism was driven by circadian rhythm-regulated metabolic patterns. These findings suggest that late-night eating may drive body fat accumulation and subsequent increased risk for metabolic disorders such as type 2 diabetes.
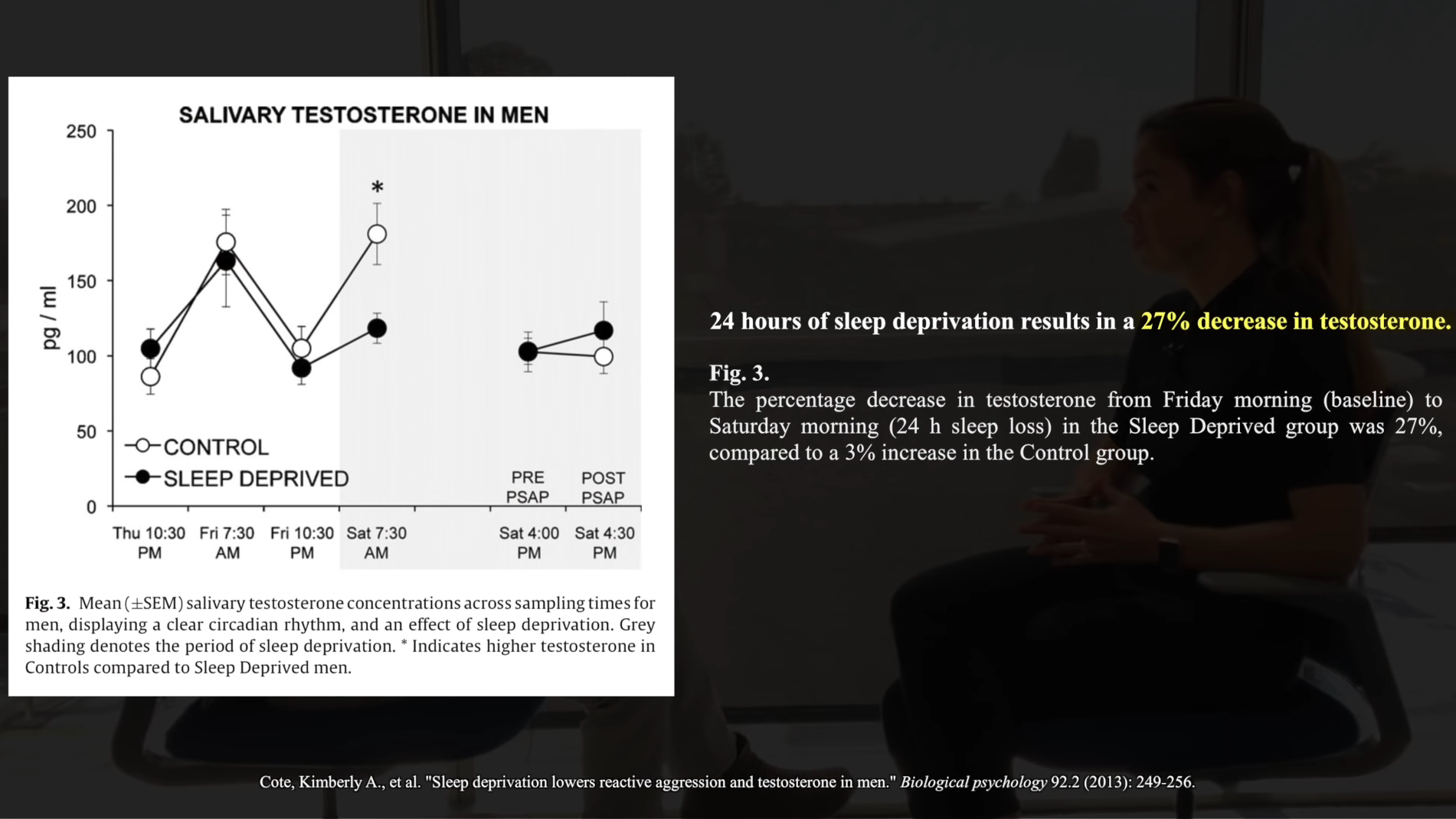
Sleep and the reproductive function: testosterone, sperm count, FSH, menstrual cycles, and fertility Testosterone in men:
- Men who only get 5-6 hrs sleep have testosterone levels of men 10 years older
- Men who sleep 5 hrs a night have smaller testicles
- Men who sleep 6 hrs or less have fewer sperm and their sperm have more deformities in the sperm
FSH and LH in women:One experiment showed:
- Women who sleep 5-6 hrs have a 20% reduction in FSH (a critical part of the reproductive pathway)
- They also have a 30% higher rate of abnormal menstrual cycles
- “From a reproductive standpoint, this is devastation.”
Sleep Loss Impairs Glucose Regulation
- Sleep restriction over several days can lead to acute insulin resistance in healthy individuals.
- Study #1: Showed that sleep restriction for 4h per night 2 nights in a row reduced the insulin response by 30% and glucose tolerance by 40% . “During the sleep-debt condition, responses were consistent with a clear impairment of carbohydrate tolerance (figure 2). The rate of glucose clearance after injection was nearly 40% slower in the sleep-debt condition than in the sleep-recovery condition. (Impact of slept debt on metabolic and endocrine function)
- Study #2: The results indicate that partial sleep restriction during only a single night reduces insulin sensitivity by 19—25% Of hepatic and peripheral glucose metabolism, as well as of peripheral lipolysis, reflected by NEFA levels. Therefore, a single night of sleep restriction to 4 h induces [acute] insulin resistance of multiple metabolic pathways in healthy subjects.
- Study #3: After 1 week of short sleep (4h per night in healthy young men) your blood sugar levels are disrupted so significantly that your doctor would classify you as pre-diabetic.
- This highlights the important role that sleep plays in glucose regulation.
- Study #4: Proposed Mechanism: We suspect the mechanisms for the reduced insulin sensitivity likely involves multiple pathways. There is evidence showing impaired insulin signaling in human adipocytes and elevated circulating free fatty acid concentration after 4 days of 4.5 hours in bed as compared to 8.5 hours in bed (41, 42). Also, inadequate pancreatic beta cell responsivity was found after prolonged (3 weeks of 5.6 hours sleep/24 hour) sleep restriction with concurrent circadian disruption (43)
- AKA the beta cells stop being as sensitive to the signal of high glucose and the cells become insensitive to signal of insulin. Now you have an inability to clear glucose on both sides of glucose equation
- HIIT training has been shown to be effective for mitigating the effects of insulin resistance in sleep deprived healthy males. So if you can’t get consistent quality sleep every day, make sure your still exercising.
Fuel Partitioning & Dieting while sleep deprived
Dietary changes when you are sleep deprived:
- Inferior fuel partitioning
- Hyperinsulinemia (means the amount of insulin in your blood is higher than what’s considered normal. Alone, it isn’t diabetes. But hyperinsulinemia is often associated with type 2 diabetes.)
- Impaired glucose disposal
- A tendency to probably eat more crap
- RQ (respiratory quotient) goes up when sleep deprived
- Respiratory quotient going up implies that under the same level of exertion, you would preferentially go after glycogen for ATP, as opposed to fat. This signals a metabolic inefficiency.
Dieting while sleep deprived efficiency
- This great study showed that dieting when underslept (6 hrs or less) was much less effective in terms of fat loss
- If underslept, 70% of what you lose is from lean muscle mass (the body holds onto fat)
- Sleep curtailment decreased the fraction of weight lost as fat by 55% (1.4 vs. 0.6 kg with 8.5 vs. 5.5-h sleep opportunity, P=0.043) and increased the loss of fat-free body mass by 60% (1.5 vs. 2.4 kg, P=0.002). This was accompanied by markers of enhanced neuroendocrine adaptation to caloric restriction, increased hunger, and a shift in relative substrate utilization towards oxidation of less fat.
- A big reason for this above is the high levels of cortisol (stress hormone) and insulin
Sleep & TestosteroneMen, who are sleeping five hours or less will have a level of testosterone which is that of someone 10 years their senior.
Sleep Deprivation on Leptin Reduction & Ghrelin Elevation
Ghrelinmakes our stomach growl.Leptinleaves us satisfied.Impact of sleep and sleep loss on neuroendocrine and metabolic function.When you are sleep-deprived, levels of leptin, which normally signal to your brain you’re full and you’re satisfied with food, that hormone is impaired by a lack of sleep. So you lose the fullness satiety signal in your brain. Downregulated leptin (the satiety hormone that signals to your brain that you are full and don’t need to eat anymore) is turned down.
Sleep Deprivation & Weight
- If you’re frequently having low levels of sleep, which is less than the recommended 7-8, you will likely see an association with this lack of sleep and weight gain. [1][2][3]
- Mortality associated with sleep duration and insomnia. Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR Arch Gen Psychiatry. 2002 Feb; 59(2):131-6.
- Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C Sleep Med. 2002 Jul; 3(4):305-14.
- Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index.Taheri S, Lin L, Austin D, Young T, Mignot E PLoS Med. 2004 Dec; 1(3):e62.
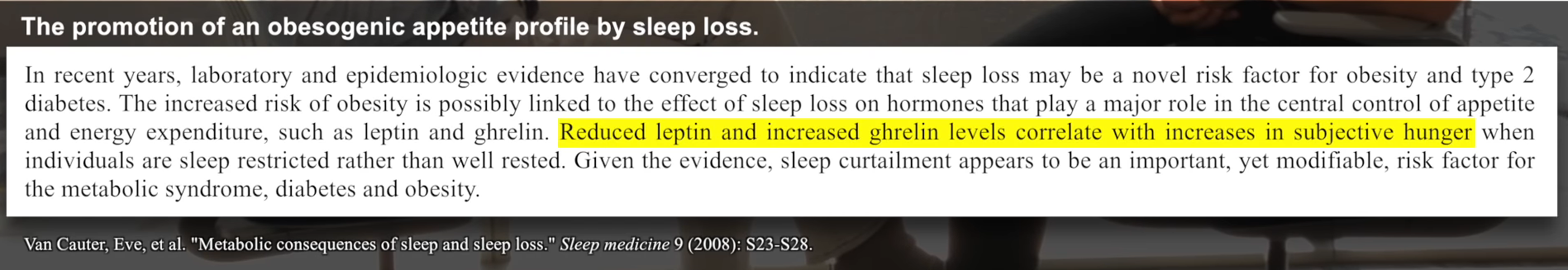
If that wasn’t bad enough, upregulated ghrelin (a hunger hormone signaling the body to eat more) is ramped up. So it’s a double whammy effect here. What does that lead to? It leads to a strong obesogenic profile of energy consumption, of food consumption.
REM Sleep dictates Leptin levels upon waking
- Higher levels of REM sleep lead to a reduction of waking leptin – this is important to note because you don’t want constantly high levels of leptin, you want functioning leptin receptors that are sensitive to leptin. Remember we discussed earlier what leptin resistance was. So, in the instance of REM sleep which is the ‘Rapid Eye Movement’ phase of sleep, most adults get a few good hours of REM [10] [11]. This allows a reduction of serum leptin while we sleep so that when we wake our receptors are sensitive and ready for this hormone once excreted. Which makes sense, we aren’t eating while we are asleep.
- Poor levels of REM sleep – leads to poor leptin sensitivity as there is no real alterations or necessary reduction in serum levels upon waking. This goes hand in hand with other studies that suggest that little amounts of REM achieved lead to lower levels of leptin, but more so in fact lower secretion as serum levels are attempted to be accounted for [12].
Ghrelin The easy way we usually associate remembering their roles in the body. These two hormones function to maintain energy homeostasis in the body when functioning correctly. Ghrelin is a peptide hormone produced by the stomach, kidneys, hypothalamus, and pituitary gland. Its purpose is to:
- Drive appetite.
- Fat production for energy storage.
- Growth of our body/growth Hormone production.
- Stimulation of Prolactin production.
- Stimulation of Adrenocorticotropic hormone (ACTH) via signaling to the pituitary gland. ACTH makes our adrenals capable of response to stress triggers and secretion of cortisol.
- Diabetogenic effect on carbohydrate metabolism, this means that it acts as an antagonist to insulin secretion/aims to suppress it.
In another recent population-based study, conducted on 1024 participants in a Wisconsin sleep cohort study; subjects found to receive less than the adequate recommended sleep value of 8 hours showed a direct increase in BMI [7][8]. This directional correlation was concluded when shorter sleep cycles habitually, showed an increase in Ghrelin levels and a decrease in Leptin. This hormonal profile ratio instigates what is commonly seen in:
- Decreased energy expenditure/fatigue.
- Higher appetite.
- Obesity/weight gain.
- The occurrence of sleep-disordered breathing among middle-aged adults.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S N Engl J Med. 1993 Apr 29; 328(17):1230-5.
- Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. Taheri S, Lin L, Austin D, Young T, Mignot EP LoS Med. 2004 Dec; 1(3):e62.
Sleep Deprivation & Increased Food Consumption
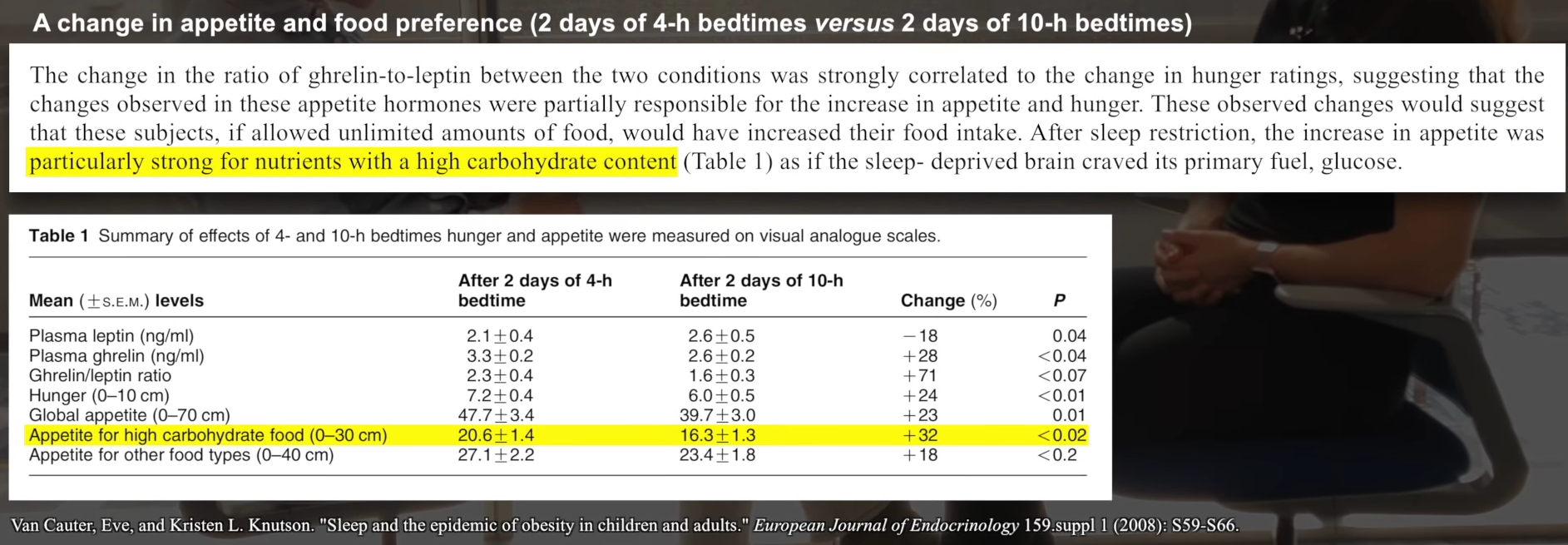
What Evan Carter discovered in her early studies was that if you give one of these sort of food buffets…and you can eat anything. It goes from, you know, sugary treats to salty treats like pretzels or potato chips to heavy-hitting starchy carbohydrates, breads, pasta, pizza all the way to salad, what you find is that you eat more of all of the food groups. But you eat mostly in terms of an increase the starchy, heavy-hitting carbohydrates as well as the sugary foods.
Sleep & Memory Consolidation:
- First, you need sleep before learning to actually get your brain ready to initially soak up new information, to initially lay down new memory traces. But you also then need to sleep after learning to take those freshly-minted memories in the brain, particularly in a region that we call the hippocampus, which you could think of almost like the informational inbox of your brain.
- But you need sleep after learning to take those new memories and then essentially hit the save button on them so that you don’t forget those informational pieces of the puzzle. So sleep before learning to get your brain ready, to acquire information. Sleep after learning to hold on to those individual facts.
- The study involved 39 healthy adults who participated in a controlled in-laboratory sleep protocol. Each of the participants experienced one night of sleep deprivation followed by two consecutive nights of recovery sleep. The authors of the study used standard recognition tests to assess the participants’ ability to form memories at baseline and every day thereafter. They used functional magnetic resonance imaging (fMRI) to assess the participants’ hippocampal functional connectivity at baseline, after sleep deprivation, and after recovery sleep.
- After a single night of sleep deprivation, the participants’ memory performance was markedly worse. Similarly, the fMRIs revealed that the participants’ hippocampal connectivity was impaired in several regions of the brain associated with memory formation. After two nights of recovery sleep, hippocampal connectivity was restored, but memory performance was still impaired.
- These findings suggest that a person needs more than two nights of recovery sleep to restore memory function after just one night of sleep loss.
Pulling an All Nighter Effect on Memory Retention (Studying & Cramming for Exams):
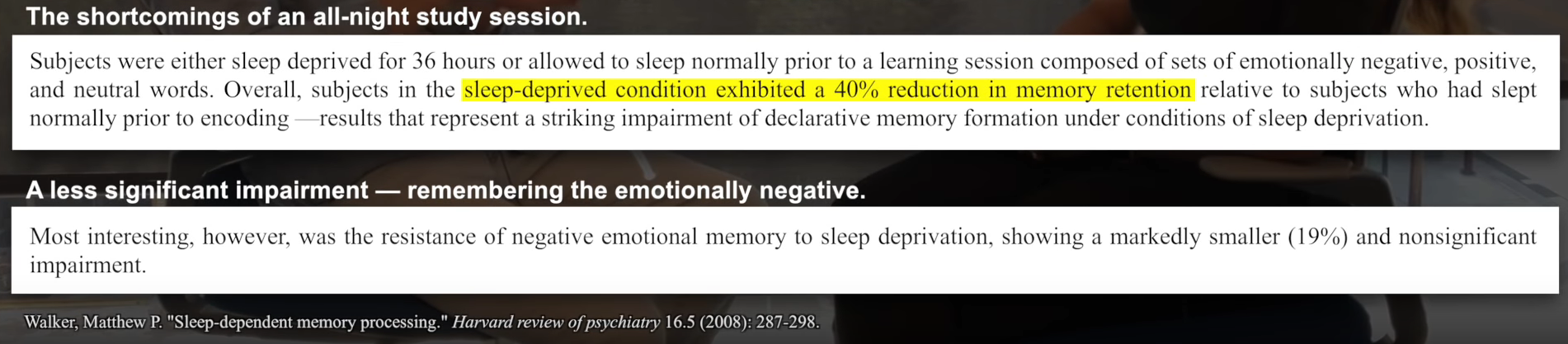
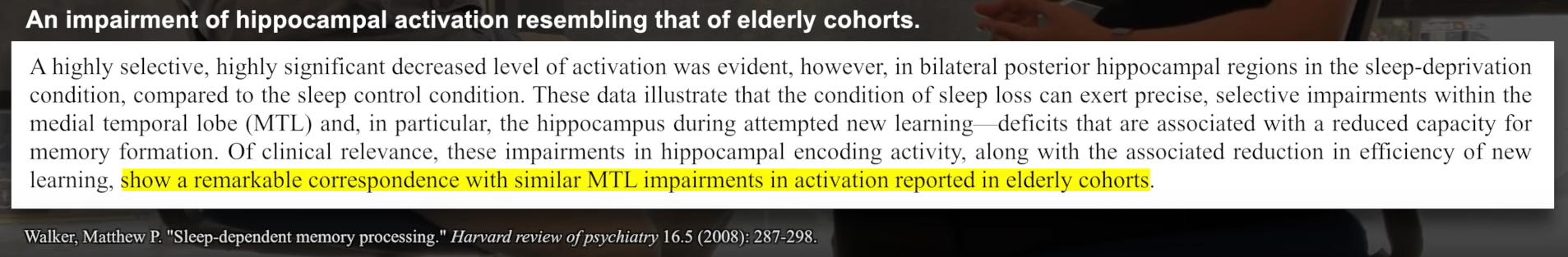
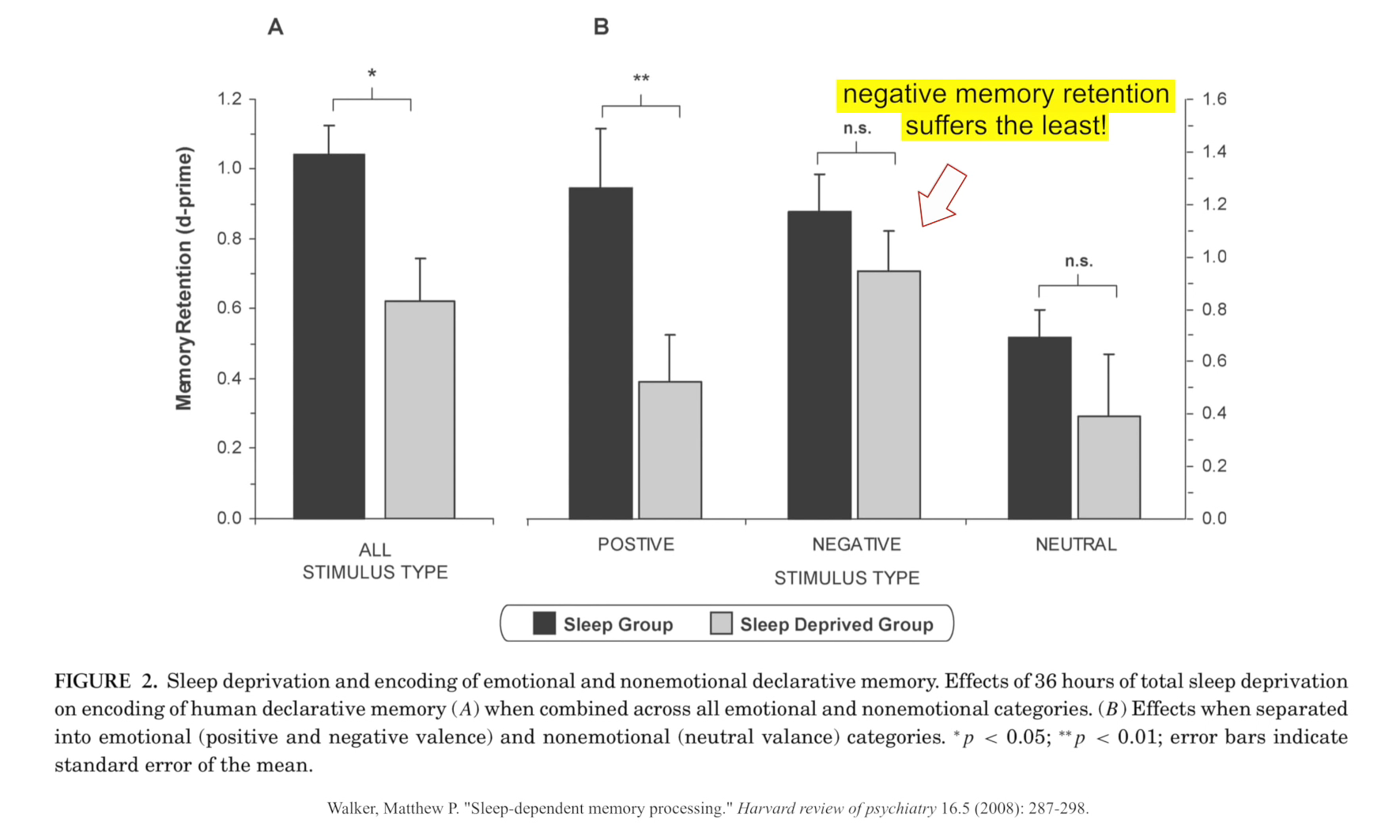
- You can’t pull the all-nighter and hope to be able to continue to learn. And we did this study. We said sort of, you know, “Is it wise to pull the all-nighter before the exam?” So we took a group of individuals, assign them to one of two groups, a sleep group and a sleep deprivation group. A sleep group, they get a full eight hours of shut-eye that we measure here at the sleep center. The deprivation group we keep awake all night under full supervision. And they don’t get any naps. There’s no caffeine.
- And then the next day, we place them inside an MRI scanner, and we had them try and learn, and cram, essentially, a whole list of new facts into the brain, into the hippocampus. And the first result was that the sleep deprivation group was about 40% more deficient in their learning ability. So they learned 40% less
- During sleep, there is a file transfer mechanism that takes place at night, that we shift memories from that short-term vulnerable storage reservoir, the hippocampus, and we move them out to the long-term storage site within the brain, which is the cortex, which essentially acts like a hard drive.
- And that means that when you wake up the next day, there are two delightful benefits. First, having shifted those memories from the short-term vulnerable reservoir to that more permanent sort of safe storage haven in the brain. They’re protected, and they’re safe, so that you’re going to remember rather than forget.
- The second benefit, however, is that sort of having cleared off those files from the hippocampus, almost like shifting files from the USB stick, you’ve cleared out all of that fresh memory encoding reservoir, so that when you wake up the next morning, you can start acquiring new files all over again.
Their theory was that the hippocampus acts like a short-term reservoir of memory that has a limited storage capacity, perhaps a little bit like a USB stick. And you have maybe, in humans, a 16-hour recording capacity for information acquisition before you have to sleep.
Sleep and cardiovascular disease
Study:Short sleep duration and incident coronary artery calcification.
- Study tracked healthy adults without signs of CVD
- By the end of the study, those getting 5 hrs of sleep or less had a 200-300% increased risk of coronary artery calcification
- The study controlled for factors like exercise, smoking, BMI, snoring, etc.
⇒ What is the mechanism?
- With lack of sleep, the body becomes much more driven by the sympathetic nervous system (the fight or flight branch of the nervous system ratchets up)
- This means more adrenaline release, high spike in cortisol levels, and blunting of growth hormone (all factors leading to atherosclerosis)
Immune System Function & Sleep Deprivation
Resource Article (Oura): How Quality Sleep Boosts Your Immune System
- Study: Take a group of healthy adults, limit them to four hours of sleep for one night, and what you see is a 70% reduction in natural killer cell activity. That is an alarming state of immune-deficiency. And it happens quickly essentially after one bad night of sleep. “imagine what it could be after months of insufficient sleep”
- So you can imagine, you know, the state of your immune system after weeks, if not years, of insufficient sleep. And it’s now the reason I think that we probably are finding, at the epidemiological level, significant links between short sleep duration, not getting enough sleep, defined as six hours or less, and your risk for the development of numerous forms of cancer.
- Individuals who reported getting <7h of sleep had almost a 3x increased likelihood of being infected by the rhino virus (common cold) relative to people getting 8h of sleep or more.
- Individuals getting 5h of sleep or less had a 70% increased risk of getting pneumonia relative to those getting 8h of sleep or more.
Sleep Deprivation & Incidence of Cold & Flu
People who were getting five hours of sleep or less in the week before they came in and were infected relative to those who are getting seven hours of sleep or more, those people who were getting five hours of sleep in the week before they got infected were four times more likely to end up developing the flu than those people who are getting seven hours or more.
Sleep Deprivation & Incidence of Flu Shot/Vaccination Effectiveness
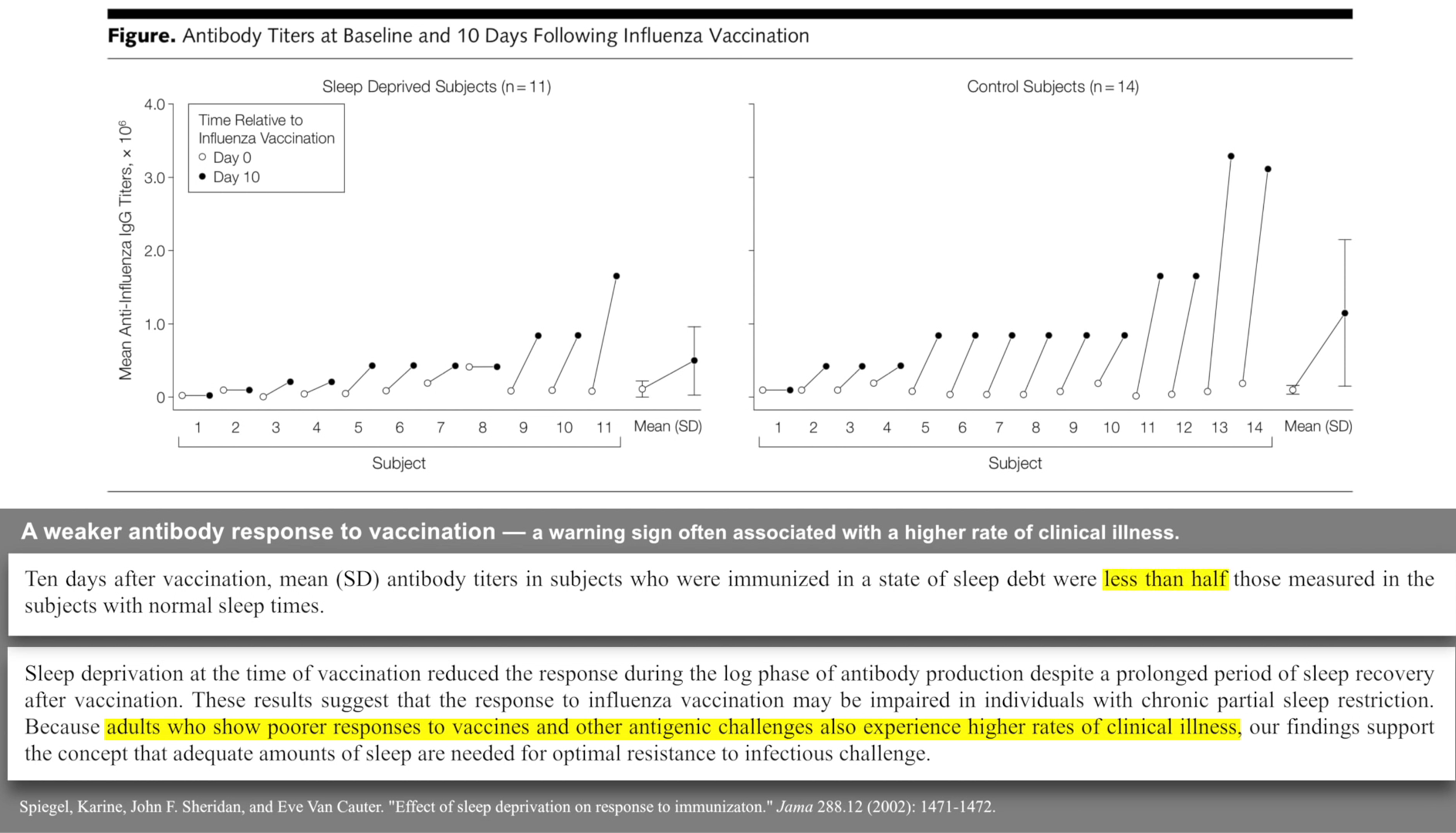
If you’re getting sort of less than five or six hours of sleep in the week before you get your flu shot, you only produce half of the normal antibody response, rendering that flu shot much less effective.
Sleep As a Carcinogen, Shift Work & Cancer
The link between the lack of sleep and cancer is now so strong that, recently, the World Health Organization decided to classify any form of nighttime shift work as a probable carcinogen. So in other words jobs, that could induce cancer because of a disruption of your sleep-wake rhythms.
Sleep and cancer development:
Significant link between sleep and cancer of bowel,prostate, and breast(3 of top 4 cancers)
- ⇒ Study using mice by David Gozal at the University of ChicagoTwo groups of mic
- Both groups have cancer
- One group got normal sleep
- Other group has their sleep restricted
- Underslept mice had tumors 200% larger than mice who slept normally
- Cancer in underslept mice had also metastasized
- The study also controlled for hypercortisolemia by having the adrenal glands removed, which means they removed the possibility that the tumor growth was fueled by hepatic glucose output by controlling for the metabolic response
- The mechanism? ⇒ Macrophage M1 cells downregulated, and M2 cells (which promote tumor growth) upregulated by lack of sleep
- ⇒ In humans…you would have both the M2 cells upregulated as well as a “tsunami” of cortisol impacting the body and driving tumor growth
Adolescences, Teenagers & School Start Times
A teenager, whose rhythm is also shifted late, you tell them to go to bed because you’ve got to wake up for early school start times, but there’s nothing they can do because their circadian rhythm has shifted forward in time. And it’s the same for owls.
- So what will happen is that they will probably stay awake for a while, then they’ll get into deep sleep. But then they have to wake up at an earlier time, and they will lose a lot of REM sleep. REM sleep, for emotional well-being, what the owls typically experience: depression, low mood, anxiety. So I think we’re really starting to put the pieces together on that component.
When you delay school start times:
- Grades improve and attendance improves according to a Seattle study
- Behavior problems drop
- Life expectancy up due to reduced car crashes
- Changed school start time from 7:35 am to 8:55 am start time change
- Car accidents dropped 70% among 16-18 year olds
- As a comparison, the invention of anti-lock brakes only dropped accidents by 20-25% and were considered a revolution
“When sleep is abundant, minds will flourish, and if our goal as educators truly is to educate, and not risk lives in the process, then I feel that we are failing our children in a quite spectacular manner, with this incessant model of early school start times.”
The sleep needs and sleep habits of teens:
- Need 9-10 hrs sleep even when 16-18 years old (Only ~11% kids get that much sleep)
- On average, teens get about 7 hrs of sleep which is a bigger relative deficit than in adults
- Teens need to go to bed later and sleep later
- Go to bed between 10 pm – midnight ⇒ sleep until 8:30 to 10:30
- But not allowed to sleep like this during week, and it’s not enough to do it on weekend
⇒ “They’re sleeping in because naturally their biological circadian rhythm, moves forward in time so they want to go to bed later and wake up later. It’s not their choice. They don’t get a choice in that. It’s biological, it’s hard wired.”
Air Temperature Importance for Sleep Quality
- For you to fall asleep and stay asleep, your body needs to drop its core temperature by about 1 degree Celsius or about sort of 2 to 3 degrees Fahrenheit. And that’s the reason that you will always find it easier to fall asleep in a room that’s too cold than too hot, because the room that’s too cold is at least taking you in the right thermal direction for good sleep.
- Historic Example: When you look at these hunter-gatherer tribes, you know, the San in Namibia, you can look at them, whose way of life hasn’t changed for thousands of years, they don’t go to bed and necessarily as immediately as the sun goes down. They usually go to bed maybe sort of 8 or 9 in the evening, several hours after sundown. But when they do start to go to bed is when the temperature drops. As the sun drops, the ambient temperature remains for a little while, and then it starts to drop, too, as the land cools, and the ambient temperature cools with the land because darkness has ensued. That seems to be a thermal trigger for them getting sleepy and falling asleep.
- So what is training us to our natural sleep rhythms is both temperature and light.
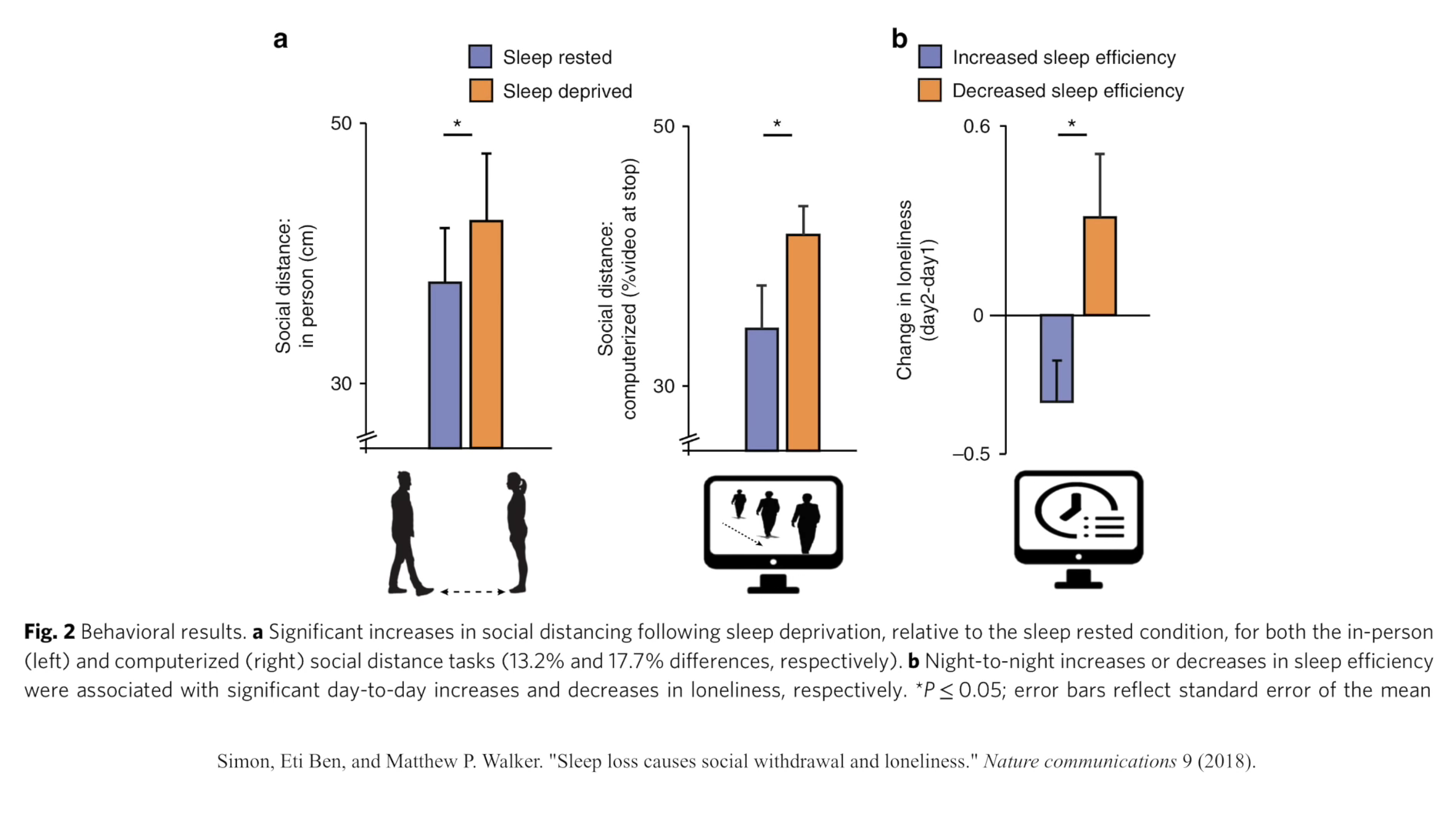
Social Behavior Tendencies, Emotion & Sleep Deprivation
- What’s interesting is that if I ask a sleep-deprived an individual to stay put, and I ask you, as an experimenter, to walk towards the sleep deprived individual, and the individual says, “Stop,” when they feel comfortable relative to when that very same individual has had a full eight-hour night of sleep. When you’re sleep-deprived, you decide to push people a further distance away from you. So you have a lower desire for social proximity and social interaction when your sleep deprived.
- Second, we then replicated that finding, but now we had them inside the MRI scanner. Because we wanted to see what was changing the brain to produce this social repulsion. What we found was that the regions of the brain that are essentially an alarm network, which is a sort of a stay-away-from-me network that is sort of in the parietal cortex and the premotor cortex, it’s sort of what we call the near space network. So it creates your comfort of boundary. And when objects start to approach you, it alarms to say, “Incoming. Be cautious. Be wary.” That part of the brain became hyperactive when people were sleep-deprived as if you were getting this repulsion signal from the brain.
Anxiety & Sleep Deprivation
It goes both ways ⇒ Mental health affects sleep, but poor sleep also affects mental healthOne single night of sleep loss can induce clinical anxiety in a person who does not normally have it
A single night of sleep deprivation increased anxiety levels by 30 percent in healthy young adults.
- The study involved 30 young adults whose brain activities and anxiety levels were measured after viewing stressful events following a sleep-deprived night versus a sleep-filled night. After the sleep-deprived night, the participants’ anxiety levels were increased after viewing the events. When the participants had a full night of sleep, however, their anxiety levels were decreased, especially for those who experienced deep sleep.
- Brain scans demonstrated that sleep deprivation among the participants impaired the activity of the brain’s prefrontal cortex, an area that mediates the effects of stress and anxiety. Conversely, deep sleep restored prefrontal cortex function, effectively restructuring the brain to reduce anxiety.
Sleep Apnea
- Heavy snoring sleep apnea is a killer. It is an outright killer. It increases your risk of basically everything you don’t want: cardiovascular disease, stroke, diabetes, and obesity. It also increases your risk of immediate death through a higher risk of car accidents.
- But one of the other problems with sleep apnea is that you don’t get the amount of deep sleep that you need. And you have hypoxic damage. Because you stopped breathing, your oxygen saturation goes down. You get hypoxia damage particularly in a region that is most sensitive to it in the brain, which is, drumroll, the hippocampus, the very same memory structure that is attacked in Alzheimer’s disease.
- So now you can see why I appeal for this sensitivity in this danger to sleep apnea. Because if you are apoe-4, you’re already at high risk of Alzheimer’s disease, you need to pay attention to your sleep. If you start snoring, and you have sleep apnea untreated, you will get less deep sleep. So you’re compromising the thing that you need to try and lower your amyloid risk to begin with, because you’re going to build up that amyloid, because you’re not going to get the amyloid clearance elsewhere in the body, for example, in the liver. And then where still the part of the brain that is attacked severely by Alzheimer’s disease and atrophies, which is the hippocampus, which is why memory fades, is a part of the brain that is damaged when you stop breathing because of oxygen desaturation.
- So, as an appeal, even if you are not apoe-4-positive, but you are snoring, or you know someone who is snoring, go and see your doctor and get a sleep apnea test. It is potentially life-saving.
Research:
A meta-analysis of the effect of media devices on sleep outcomes
- The American Academy of Pediatrics highlight factors such as electronic media device use, early school start times and increasing caffeine consumption, contribute substantially to this trend of insufficient and deteriorating sleep in the pediatric population (4, 5).
- 72% of all children and 89% of adolescents have at least one device in their sleeping environment, and most are used near bedtime (3, 6).
- Such devices are hypothesized to adversely impact sleep through a variety of pathways (7, 8). First, they may negatively affect sleep through directly displacing, delaying or interrupting sleep time. Second, the content can be psychologically stimulating, and finally the light-emitted from devices impact circadian timing, sleep physiology, and alertness (9).
- Bedtime access and use of media devices was significantly associated with inadequate sleep quantity; poor sleep quality; and excessive daytime sleepiness.
Sleep problems: predictor or outcome of media use among emerging adults at university?
- Higher media use has been consistently associated with more irregular sleep patterns, shorter sleep duration, as well as more sleep problems (Chahal et al., 2013; Choi et al., 2009; Oka et al., 2008; Punamäki et al., 2007). Researchers have proposed that increased media use may be linked to poor sleep because time spent engaged in media use may directly displace sleep (Li et al., 2007; Oka et al., 2008; Owens et al., 1999; Van den Bulck, 2004; Zimmerman, 2008). Highly arousing media content (e.g. a violent movie) also may lead to nightmares and poor overall sleep quality (Li et al., 2007; Owens et al., 1999; Zimmerman, 2008), particularly among individuals whose emotion regulation strategies are not yet fully developed.
Analysis of circadian properties and healthy levels of blue light from smartphones at night.
- The daily production of melatonin can be rapidly suppressed by exposure to blue light, either by short pulses or prolonged illumination, with the short (blue) wavelengths being much more effective than longer wavelengths (red to yellow) in inducing this response10. Recently, Falchi et al. reported that blue light from artificial light alters natural processes, interferes with melatonin production, and disrupts the circadian rhythm11. Consequently, exposure to blue light from artificial light sources, such as a blue-enriched LED lamp, LED backlight for liquid crystal displays (LCDs), and organic light-emitting diodes (OLEDs), late in the evening and at night could be detrimental to human health12–15. In addition, it was also reported that blue light has a greater tendency to affect living organisms by disrupting biological processes that rely on natural cycles of day and night16–18. Therefore, light rich in short-wavelength (blue) light should be avoided in the late evening to promote a healthy night-time lighting environment. Managing the light in artificial light sources for optimum health and well-being in a bright night environment is thus critical.
Sleep duration may influence children’s mental health.
- Method: The authors of the study analyzed structural MRI data from more than 11,000 children between the ages of nine and 11 years who were enrolled in the Adolescent Brain Cognitive Development (ABCD) Study. They also assessed the children’s cognitive performance and mental health status. The parents of the children in the study provided information about their child’s sleep duration by answering the question, “How many hours of sleep does your child get on most nights?”
- The study revealed that children who had shorter sleep duration were more likely to experience depression and anxiety and were more likely to exhibit impulsive behavior and poor cognitive performance. The association between poor sleep and depression persisted and was observed at the one-year follow-up. In addition, the volume of the orbitofrontal cortex, prefrontal and temporal cortex, precuneus, and supramarginal gyrus regions of the sleep-deprived children’s brains were lower than children who received adequate sleep.
Blue Light
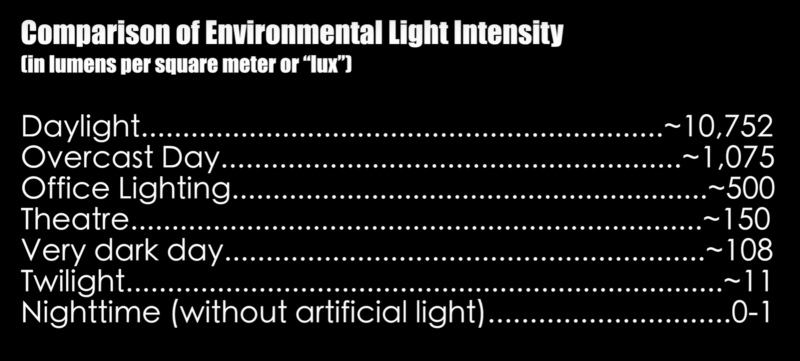
- Harvard researchers and their colleagues conducted an experiment comparing the effects of 6.5 hours of exposure to blue light, versus exposure to green light of comparable brightness. They found that blue light suppressed melatonin for about twice as long as the green light and shifted circadian rhythms by twice as much (3 hours compared with 1.5 hours). And worse, it’s been linked in recent studies to an increased risk of obesity and some cancers
Blue Light During The Morning/Day
- “What I’ve found though is something a lot of people don’t go out of their way to emphasize is exposure to as much natural blue light as possible early in the day, getting your ass outdoors as soon as possible in the morning when the sun has come up and exposing yourself to sunlight early in the day. That was one of the most profound things I’ve done in the past two years to increase my deep sleep percentages is my blue light exposure early in the day, preferably to as wide a spectrum of light as possible.” – Ben Greenfield
Blue Blocking Glasses
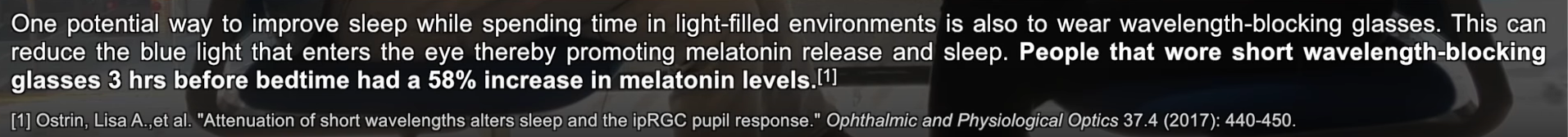
2 People who wore blue wavelength-blocking glasses while still using their digital devices had a 58% increase in their night time melatonin levelsWaking Up Before Sunrise:Your circadian rhyme starts in the morning and if you get up before the sun is up put blue blockers on. That stimulates what our ancestors would have done with waking up to the sunrise which is always red then yellow so once the sun has come up more to yellow then take them off. So you jump start your circadian rhythm at the right time and ease yourself into it.
iPhone/iPad and television usage⇒ Biological reasons to avoid electronics…
- This study suggests using an iPad before bed has negative effect on sleep ⇒ 50% drop in melatonin (aka you lose 50% signal of sleep timing), and your peak melatonin will arphillrive 3 ”
- iPad time also reduces REM time
- Effects last 2-3 days
- Television ⇒ TV doesn’t have quite the same effect, but… it does make brain associate bedroom with TV and “when you start to form those maladaptive associations, it can be a trigger of insomnia and anxiety.
Developing Children Are More Sensitive to Light Than Adults
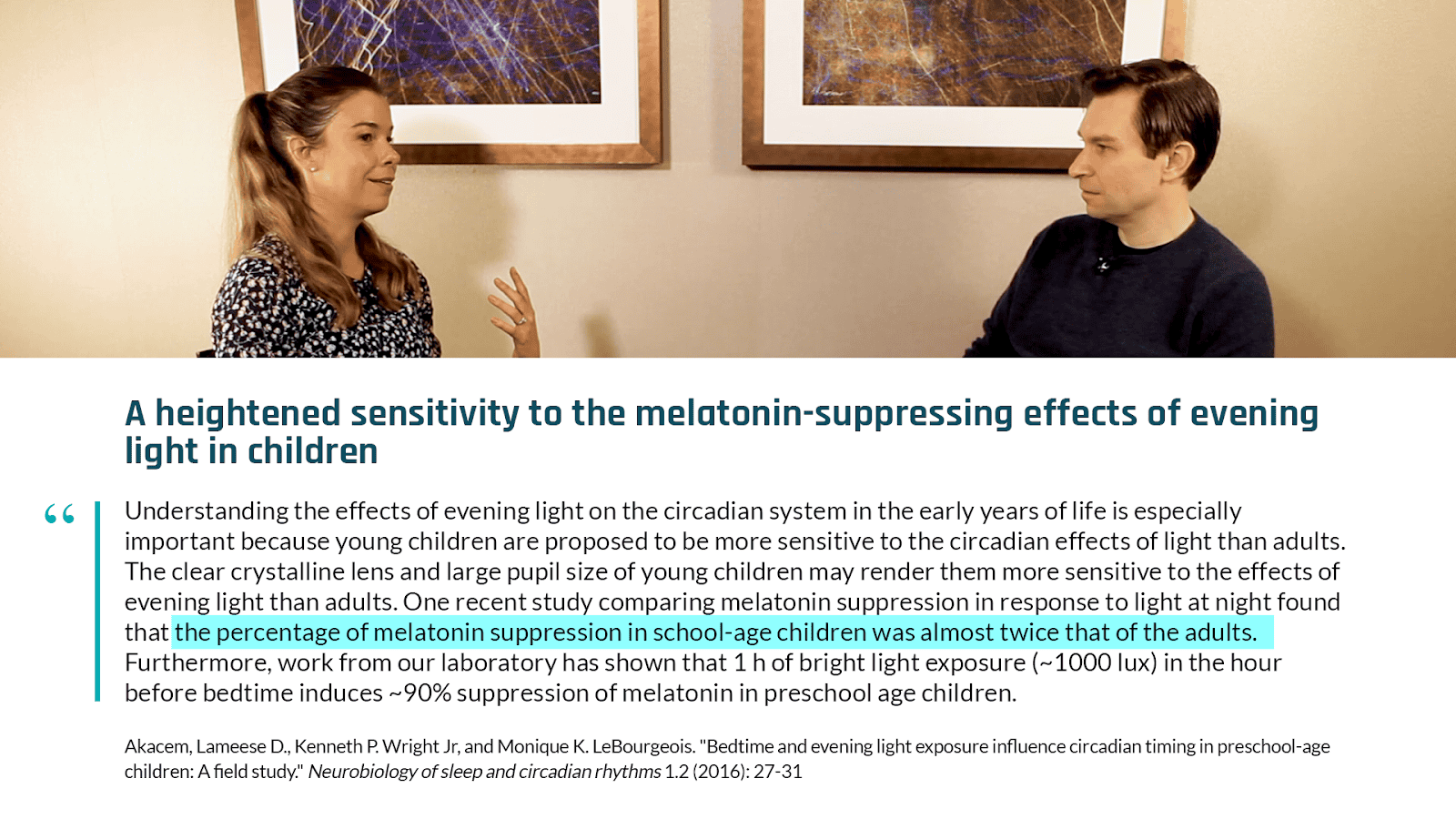
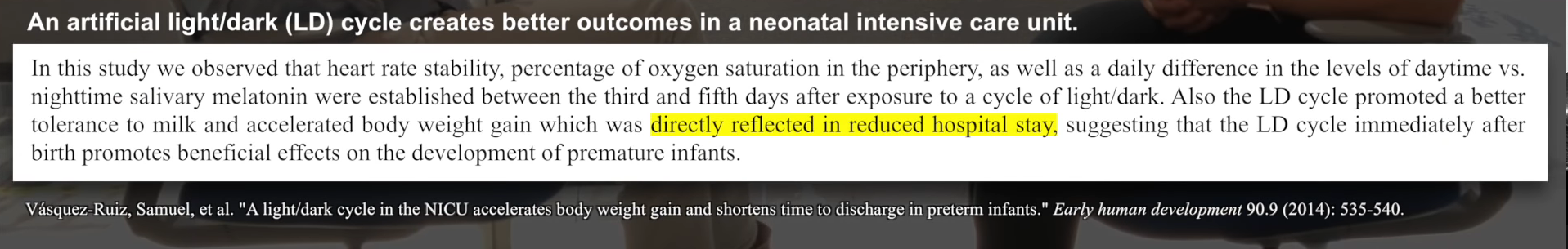
Neonatel Intensive Care Unit: Babies Circadian Rhythm & Light
- So in the neonatal intensive care unit, what we used to have when we go in there, you just have constant light on all of the time, dim light on 24 hours a day, which prevented those infants getting the signal of a regulating 24-hour light-dark cycle.
- If you regularized light in the neonatal intensive care unit, so light during the day, darkness at night, in these studies, what you see is basically almost a 50% to 60% increase in oxygen saturation within the blood of these neonates in the intensive care unit. Weight gain increases dramatically. And they end up exiting the neonatal intensive care unit at about 2-2.5 weeks earlier than they would otherwise.
Mathew Walker on Joe Rogan Notes:
Professor of Neuroscience and Psychology at the University of California, Berkeley, and Founder and Director of the Center for Human Sleep Science.
- Your body doesn’t function as effectively through nrem stage 3-4 where most of the deep sleep occurs when you’re in unfamiliar locations like hotels because of this evolutionary threat detection system that inhibits half your brain from entering stage 3-4 instead staying in the lighter stages as your body stays on guard to threats.
- Men who sleep 5-6 hours a night will have the testosterone of those 10 years their senior.
- Having less sleep increases all cause mortality. The irony is people want to sleep less so they can accomplish more exclaiming how ‘short life is’ – well its going to be even shorter if you sleep less. The old maxim you can sleep when your dead is mortally unwise advice because we know from the data you will be dead sooner and the quality of that life will be worse.
- Insufficient sleep across a lifesapen seems to be one of the significant lifestyle factors that determine whether you’ll determine Alzheimers.
- Gallup did a pole in 1942 and found the average American adult was sleeping 7.9 hours p/n and now that number is down to 6 hours and 31 minutes for average adult in America.
- The number of people that can survive on <6 hours of sleep without showing any impairment is 0% (rounded down). However there’s a small fraction of 1% of the population that has this gene that allows them to survive on 5 hours of sleep that helps maintain wake fullness.
- In the spring (US) when we lose an hour of sleep we see a subsequent 24% increase in heart attacks and in the fall when we gain an hour back we see a 21% decrease in heart attacks – its bidirectional – thats how fragile your body is to even the smallest change in sleep.
- One study they took a group of healthy adults and limited them to 6 hours of sleep p/n and compared the gene activity to when they were getting 8h p/n. Results = 711 genes were distorted in their activity caused by 1 week of 6 hours of sleep, about half of those genes were increased /over expressed in their activity (inflammatory genes) and the other half were decreased which were responsible for immune support
- Doctors on average have only 2~ hours of sleep education in the medical curriculum
- If your dieting but not getting sufficient sleep 70% of all the weight you lose will come from lean body mass (muscle) and not fat. Your body becomes stingy about the way it oxidizes fuel when under slept.
Shift Workers:
- Linked to higher rates of obesity, diabetes and cancer.
- Now the WHO has classified any form of night time shift work as a probable carcinogen (capable of causing cancer).
Sleep & Performance
- Effect of sleep deprivation on tolerance of prolonged exercise: If your getting 6 hours or less of sleep your time to physical exhaustion drops by 15 to 40%. Lactic acid builds up quicker and your ability to inspire O2 and expire CO2 decreases.
- heavy exercise performance after 36 h without sleep was compared with that after normal sleep in eight subjects. During prolonged treadmill walking at about 80% of the VO2 max, sleep loss reduced work time to exhaustion by an average of 11%. four showed less than a 5% change in performance after sleep loss, while four others showed decrements in exercise tolerance ranging from 15 to 40%.
- They notice obvious impairment in brain function at 7 or less hours sleep.
The Effects of Sleep Extension on the Athletic Performance of Collegiate Basketball Players (2011)
- Sample: Eleven healthy students on the Stanford University men’s varsity basketball team (mean age 19.4 ± 1.4 years).
- Design: Subjects maintained their habitual sleep-wake patterns for a 2–4 week baseline period during the NCAA basketball season and stayed within the limits of 6–9 h of subjective sleep time each night. Subjects then extended their nocturnal sleep duration for 5–7 weeks during which they obtained as much extra sleep as possible with a minimum goal of 10 h in bed per night.
- they estimated they slept eight hours but averaged about 6 hours and 45 minutes. While trying to sleep 10 hours during the second part of the study, they actually achieved about 8 1/2 hours.
- Results: Total objective nightly sleep time increased during sleep extension compared to baseline by 110.9 ± 79.7 min (P < 0.001). Subjects demonstrated a faster timed sprint following sleep extension (16.2 ± 0.61 sec at baseline vs. 15.5 ± 0.54 sec at end of sleep extension, P < 0.001). Shooting accuracy improved, with free throw percentage increasing by 9% and 3-point field goal percentage increasing by 9.2% (P < 0.001). Mean PVT reaction time and Epworth Sleepiness Scale scores decreased following sleep extension (P < 0.01). POMS scores improved with increased vigor and decreased fatigue subscales (P < 0.001). Subjects also reported improved overall ratings of physical and mental well-being during practices and games.
Things affected by insufficient sleep in drivers/athletes
- Spatial attention: Matthew says something called “spatial attention” goes down very quickly under conditions of sleep deprivation
- Quick decision making: When other racers are on the track, it becomes strategic and you have to make multiple decisions in split seconds, and sleep affects critical components of that
- Judgement: It’s incredible how much your judgment can be impaired when others are on the track probably due to sleep’s impact on impatience and impulsivity (can lead to irrational thinking)
- Most world records are broken at the Olympics during the peak of most circadian rhythm (about 1 or 2 in the afternoon)
- HGH is also a naturally occurring hormone in the body that tends to spike in the afternoon and early evening. The hormone generally peaks overall when people are sleeping.
- While there is a peak time of day for performance, there is also a mirror time when athletes will be far from their best. A study published this March in the medical journal Chronobiology International said events scheduled late into the night in the Summer Olympics could “lead to injury and may compromise an athlete’s decision-making, attentional, physiological and other processes.”
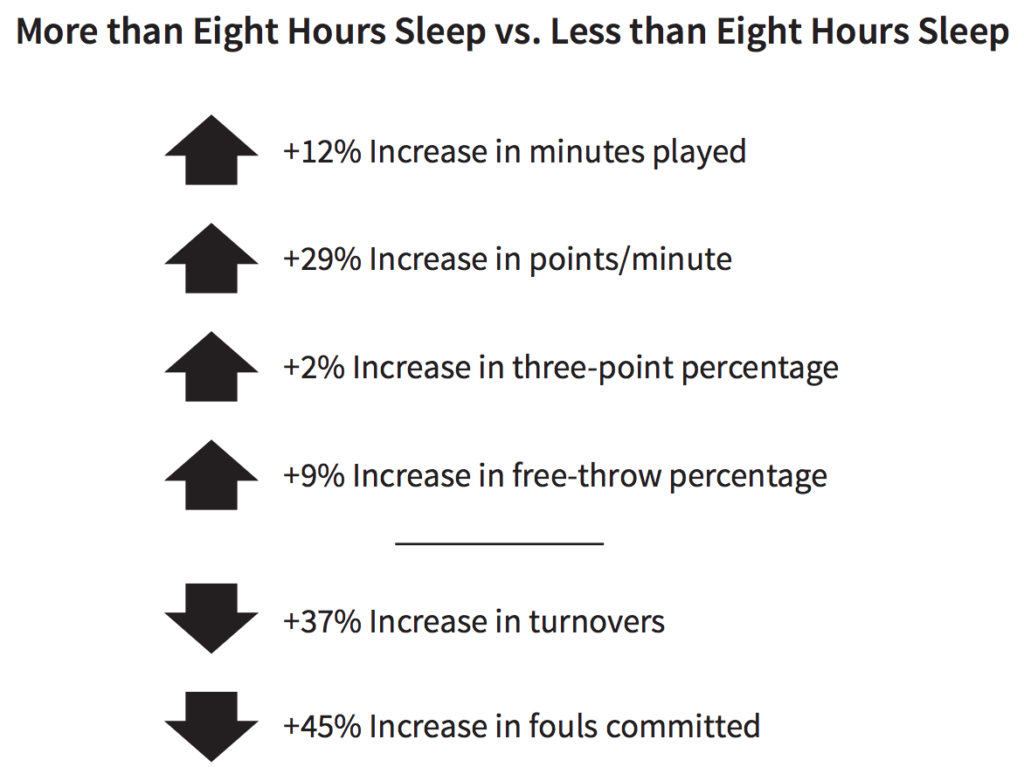
Figure 4. NBA player performance. Image credit: Why We Sleep
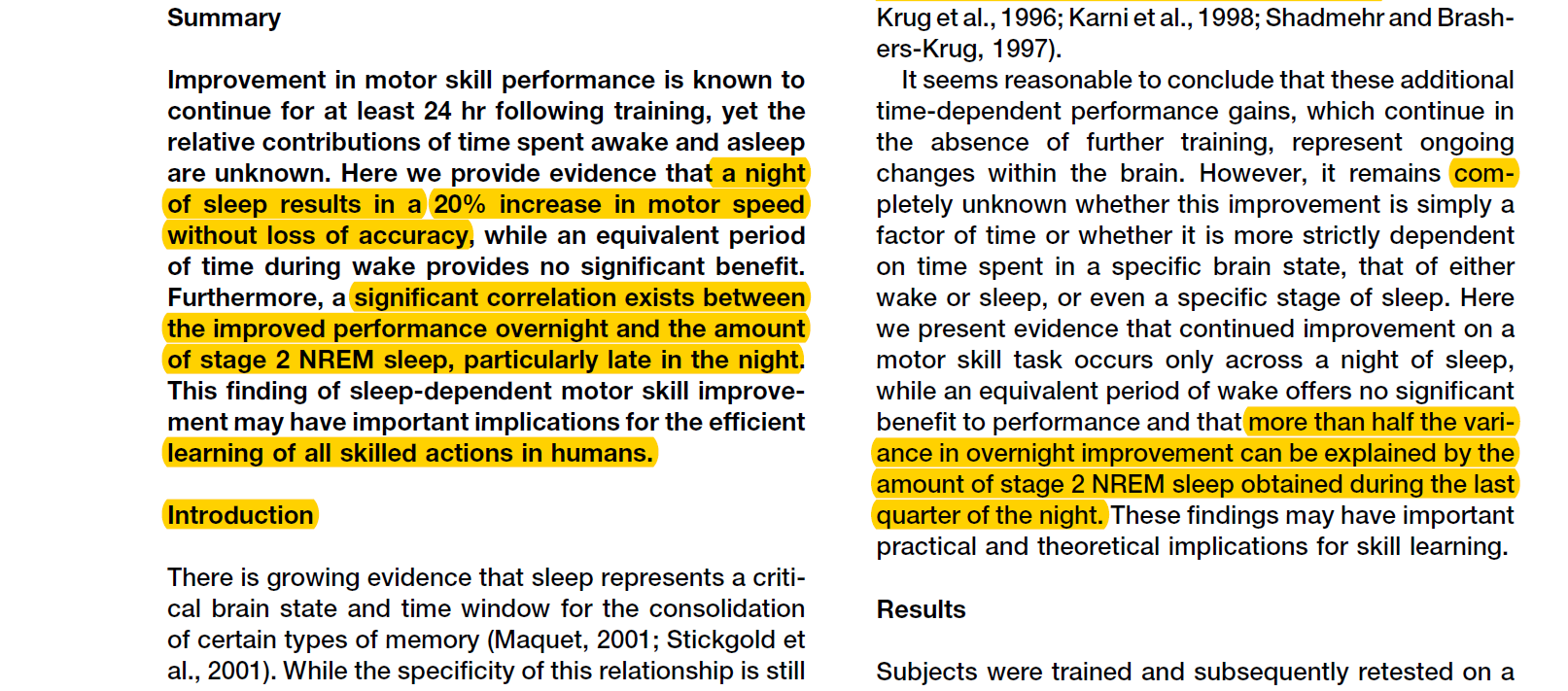
Sleep for refinement of motor skills:
- When learning a new motor skill and learning new navigational pathways your brain fires in a parcticular sequence according to the movement. During sleep the brain is replaying the same memory sequence it was learning whilst it was awake but at a speed that is 20x faster to help scuplt the skill and evcen improve it.
- “practice does not make perfect – practice with a good night of sleep makes perfect because you come back the next day and your 20-30% better in terms of your skilled performance than where you were at the end of your pracitce session the day before.”
- Study: Practice with Sleep Makes Perfect Sleep-Dependent Motor Skill Learning:
Sleep & Injury
- The less sleep you have the higher your injury risk – it’s a linear relationship. Almost a 60% increase in probability of injury risk during a season in 9 hours vs 5 hours sleep.
Drowsy Driving:
- After 20 hours of being awake you are as impaired cognitively as you would be if you’re legally drunk (US).
- Kills more people than either alcohol and drugs combined. When you’re underslept you start to have whats called micro sleeps where your eyelid partially closes and your brain goes to sleep for a very brief amount of time. Problem with drugs and aclohol is that you get a later reaction time, drowsiness = no reaction.
- If you have to drive at night and are falling asleep wet your face with water.
- A school in wyoming shifted their school start from 7:35AM to 8:55AM and they fund a 70% reduction in car accidents the next year in that area. Here’s a simple biological factor that will make people safer while improving cognitive function as well due to more sleep in kids.
- A school in edina minnesota changed school start times form 7:25AM – 8:30AM. Before they changed it the top 10% performing students got an SAT score of 1288 and the following year after the change was 1500. A huge increase.
Sleep Deprivation/Sleep Debt:
- Your brain has no capacity to regain all the sleep its lost in one night. You will sleep longer given the freedom to, post sleep deprivation but you will only get back 30-50% of the total lost hours. Sleep is not like the bank, you cant accumulate a debt and hope to pay it off on the weekend – there’s no credit system for sleep.
Can you “sleep off” your sleep debt over the weekend?
- People think they can accumulate sleep debt during week and then make it up on weekend (“social jet lag”)
- It’s like sleep bulimia (with binging and purging)
- It’s torture on circadian biology to drag body clock by 3 hours every weekend (“It’s like flying from San Francisco to New York every weekend.”)
Gene Variation That May Protect Some From Sleep Deprivation
The p.Tyr362H is a variant of the BHLHE41 gene allows some people to m,aintain normal alterness and show limited signs of inflammation on less sleep compared to their twin counterpart who didn’t have that gene. But this genetic variation is rare.
- Gene mutation the real secret for successful short sleepers
- Study of twins discovers gene mutation linked to short sleep duration
How to Correct Sleep Problems
- exogenous agents like melatonin
- Blue light
- regular exercise
- exposure to daylight as soon as you wake
- manipulations of body temp like contrast therapy (hot / cold) to stimulate drowsiness
Is it harmful to read in bed with a nightlight?
- If you struggle with sleep (either sleep onset or maintenance insomnia), you should read in different room and go to bed when sleepy
- The brain is associative ⇒ to break association, get up and go somewhere else an only go back to bed when get sleepy
- You wouldn’t sit at table waiting to get hungry, so stop lying in bed waiting to get sleepy
Practical Way’s to Dramatically Improve Sleep: Basic Sleep Hygiene
10-3-2-1-010 – The hours prior to sleep in which you will not drink caffeine.3 – The hours prior to sleep in which you will not eat or drink anything other than water.2 – The hours prior to sleep in which you will not work.1 – The hours prior to sleep in which you will not be exposed to screens.0 – The number of times you hit the snooze button.
Summary:
1. Regularity of wake and sleep consistent within 1h each night 2. PITCH BLACK room. Including any electronic LED lights . All electronics switched off that emit EMF. Use a eye mask ideally because usually no one can make a pitch black room. 3. No sound. Use ear plugs if necessary or white noise from a fan, water fountain, rain sound app. 4. Make room as cold as possible. 16-19 degrees. 4. Eliminate blue light 30min minimum..ideally 1h before sleep. Use blue blockers. Use red light globe and candles in your room. No fluorescent lighting. It will blunt and delay melatonin release. 5. Develop a downregulation routine that doesn’t involve electronic devices ideally 30m before. Could be soft tissue release routine with some light fiction reading and meditating. 6. If you pee during the night try no fluid intake 1h before sleep. 7. Caffeine has a quarter life of 12h which can reduce NREM sleep and onset to sleep. *Also depends how you metabolised caffeine – fast/slow/moderate metaboliser of caffeine
- Regularity waking up and falling sleep at a similar time. +-1 hour.
- Darkness & Light Pollution:
- You really do need some degree of darkness at night to release that hormone melatonin, which helps trigger the timing of the healthy onset of sleep. 3-4 hours is the time to start thinking about your light saturation exposure, certainly in the last hour before bed. E.G. f.lux
- Anxiety: So I think light is a feature, but I also think part of the problem with computers and iPads and iPhones is they do trigger anxiety. They are what I would describe as anxiogenic pieces of hardware. Most people get a lot of their anxiety infusion in part through these devices.
- Upon sunset Switch off half the lights in the house and dim all lights to stimulate melatonin
- 1 hour of iPad reading vs 1 hour of reading a book in dim light can delay the release of melatonin by 3~ hours so your melatonin peak isn’t going to arrive til 3 hours. And you don’t get the same amount of REM sleep and you wake up not as refreshed and restored as a result of the lower melatonin release affecting your REM sleep.
- Temperature: Keep it cool. 63 (17C) to 66 (18C) degrees for most people is optimal
- Your brain needs to drop it’s temp by 2-3 F (~0.5C) to initiate sleep and the reason why you’ll always find it easier to sleep in a room that’s too cold compared to too hot. Makes people fall asleep faster and deeper NREM sleep. Sleeping naked also seems to help. The paradox here is that you need to warm your feet and hands to help move the blood away from your core out to the surface and radiate that heat. Or have a hot bath/shower – you dont fall asleep faster because you feel all warm and toasty, in the bath you get vasodilation and you get out of the bath and you have this massive thermal dump of heat that evacuates from the body = your core temp goes down so you can sleep easier.
- Reducing fluid intake – related to sleep disturbance and inflammation. The more you wake up in the middle of the night to use the restroom, the higher the likelihood of developing some low-grade inflammation or worse
- Don’t Stay in Bed Awake
- I think more than 20 minutes is not great, because what happens is that your brain very quickly starts to learn the association between being in bed is about being awake rather than your bed being the place of sleep. And so it learns this association.
- And so many of the patients that speak to, they’ll say, “Look, you know, I’m falling asleep on the couch watching television, and then I get into bed and I’m wide awake, and I don’t know why.” And the answer is because you’ve made the association between your bed is the place of wakefulness, not your place of sleep. So the answer is you need to break that association. Get out of bed, go to another room, in dim light, just read a book, no computers, and only return to bed when you feel very sleepy.
- And the first night this may mean that you’re awake for two or three hours. And it sounds bad, and it sounds strange coming from someone like me, but that’s better than staying in bed awake for those two or three hours. And over time, gradually, by only returning bed when you’re sleepy, your brain will relearn the association that it once had when you’re a child, and you can relearn it, which is that your bed is a place of deep sleep and sound sleep.
- Caffeine
- It’s what we call psychoactive stimulant. It’s the only psychoactive stimulant, by the way, that we readily give to our children in an unregularized free way, which I think is a problem. Caffeine has several problems with it. Firstly, because of it being a stimulant, it can keep you awake and it makes it harder for you to fall asleep.
- Caffeine blocks adenosine receptors in the brain ⇒ it’s hitting the “mute button” on sleepiness
- Caffeine has a half-life of 6 hours
- And a quarter life of 12 hours
- So if you drink a full cup of coffee at noon, quarter of that caffeine is still in the brain at midnight
- It’s like drinking a quarter of a cup of coffee right before bed
- Even for people who say they sleep just fine after consuming caffeine, one study showed that 200 mg of caffeine before bed resulted in a 20% reduction in deep sleep (the same as aging you 20 or 30 years to get the same drop)
- “Look, I’m one of those people who can have a cup of coffee with dinner and I fall asleep and I stay asleep, and I’m just fine.” Even if that’s true, we and others have done these studies, if you give someone a standard dose of one cup of coffee in the evening, 200 milligrams of caffeine, the amount of deep sleep that they have is reduced by 20%. You would normally have to age an individual by 10 or 15 years to drop your deep sleep quality by 20%, or you can do it simply by having a cup of caffeinated drink or coffee in the evening. So caffeine is a problem.
- The other problem with caffeine is its duration of action. Caffeine has a half-life of about six or seven hours. And a half-life simply means the amount of time it takes for a 50% of the drug to still be in your system or 50% of it to be cleared. Caffeine has a quarter life of about 12 hours. In other words, if you have a cup of coffee at noon, a quarter of that caffeine is still circulating in your brain at midnight.
- So the advice would be try to cut caffeine off around about midday if you can. And even if you’re someone who, you know, can fall asleep fine, stay asleep, you should just know that caffeine can still impact your deep sleep.
- The Caffeine Cycle: It’s what usually creates the vicious cycle, by the way, that those people will wake up the next day, they feel unrefreshed and unrestored by their sleep, they don’t remember waking up, so they don’t think it’s the cup of coffee, but now they start reaching for two cups of coffee in the morning rather than one. They’ve got now more caffeine in the system. The next night, they have even less deep sleep. The next morning, they wake up even less refreshed. And now they drink more caffeine. Self-fulfilling prophecy.
- Alcohol
- Alcohol is a sedative. It’s a class of drugs that we call the sedatives. And sedation is not sleep. So when you drink alcohol, what you’re doing is sedating your cortex. You’re just knocking yourself out. And that’s why you think that you fall asleep faster.
- alcohol fragments sleep so you wake up many more times during the night; often so brief that you don’t remember but they have an impact on your physiology So this comes back to the third of the four pillars of good sleep, which is continuity. It takes away your continuous asleep, and it makes it fragmented.
- alcohol blocks REM sleep, so you wake up unrefreshed and unrestored
- THC & CBD
- Cannabis, Cannabinoids, and Sleep: a Review of the Literature.
- Delta-9 tetrahydrocannabinol (THC) may decrease sleep latency but could impair sleep quality long-term. Novel studies investigating cannabinoids and obstructive sleep apnea suggest that synthetic cannabinoids such as nabilone and dronabinol may have short-term benefit for sleep apnea due to their modulatory effects on serotonin-mediated apneas. CBD may hold promise for REM sleep behavior disorder and excessive daytime sleepiness, while nabilone may reduce nightmares associated with PTSD and may improve sleep among patients with chronic pain. Research on cannabis and sleep is in its infancy and has yielded mixed results. Additional controlled and longitudinal research is critical to advance our understanding of research and clinical implications.
- THC: So this comes back to the third of the four pillars of good sleep, which is continuity. It takes away your continuous asleep, and it fragmented. The final part of alcohol is that it’s one of the best chemicals that we know for suppressing REM sleep alongside marijuana. Now, by the way, I should say that’s THC-specific. If you look at CBD, the evidence seems to be less clear. CBD actually doesn’t seem to be as detrimental to your sleep as THC.
- THC does tend to decrease the time it takes you to fall asleep, but it tends to make you sometimes wake up more throughout the night, but it certainly does seem to block REM sleep.
- One of the other problems with THC dosing of sleep is that you become dependent on that for sleep. And when you stop using THC for sleep, you have quite bad rebound insomnia, which leads to then a perpetuating cycle of dependency.
- CBD: High-dose CBD seems to help people sleep more consistently. Now we don’t know about the dependency. We don’t know about the long-term effects.
- What the early data on CBD is showing:
- Falling asleep faster with CBD
- Early tentative preliminary evidence suggests it does not have the same negative impact on REM
- CBD might also benefit some sleep disorders: Might reduce severity of sleep apnea and Might also help PTSD-related sleep problems
- It’s dose dependent, and it’s not clear at this point what the optimal dose is
- There may be other doses that are actually detrimental to sleep and we need to stay away from them
- So it might that there is a U-curve with a “sweet spot” for dosing with other doses being detrimental to sleep
- Cannabis, Cannabinoids, and Sleep: a Review of the Literature.
- Supplements & Herbs:
- Use herbal therapies – try passionflower, or 320 mg to 480 mg of valerian (valeriana officinalis) root extract standardized to 0.2 percent valerenic acid one hour before bed.
- Take 200 to 400 mg of magnesium citrate or glycinate before bed – this relaxes the nervous system and muscles.
- Other supplements and herbs can be helpful in getting some shuteye – try calcium, theanine (an amino acid from green tea), GABA, 5-HTP, melatonin, and magnolia.
- Supplement Sleep Stack (William Wallace, PhD)
- Magnesium (I like to mix L-threonate and bisglycinate) -2g of threonate contains 140-150mg of elemental. 2g of glycinate should yield 200mg of elemental. Glycinate is the cheaper option but still effective – magnesium is a cofactor in melatonin production that not only helps synthesize it but helps regulate the right levels of it.
- B6 (p5p) – 10-50mg. p5p is basically the active version of B6. It helps optimize cortisol (aiding in its synthesis and breakdown), making it easier to wake up from sleep. It is also helpful for getting to sleep, as it aids tryptophan in its conversion to serotonin (thus, more serotonin available for melatonin synthesis).
- Tryptophan – 1-2g – The essential amino acid responsible for synthesizing serotonin. Higher levels of tryptophan and serotonin at night will likely aid in higher levels of melatonin, as serotonin converts to melatonin downstream. I like tryptophan over 5-htp, as many people can’t handle 5-htp well and its conversion to serotonin in the brain is poor unless supplemented alongside other ingredients (plus the research advocating for its use isn’t good but if you prefer it, have at it).
- Glycine – 3-6g – One of the two primary inhibitory neurotransmitters (next to GABA). Glycine neurons are largely classified as interneurons (as interneurons are mostly inhibitory) and found heavily in the spinal cord but also the brian.
- Multifarious Beneficial Effect of Nonessential Amino Acid, Glycine: A Review
- If you find yourself in a situation where you’ve got to eat something close to bedtime, glycine-rich gelatin is a great option because glycine has been shown to enhance the quality of your sleep
- Inositol – 1-2g – Formerly classified as vitamin B8, inositol enhances the effect and efficiency of neuronal communication in the brain (particularly, serotonin signaling), as it anchors signaling proteins to neurons.
- https://au.atpscience.com/product/adrenal-rx/ (Jess found this really helped her a lot)
Visual Overwriting – The Simpsons Method (Short & Uplifting Episodic Entertainment Television) #Post
- Visual overwriting is a term from Tim Ferris to crowd out any replaying mental loops and distractions that will inhibit sleep (e.g. thoughts of, what should I do, what will I do, what have I done, to-do lists, arguments etc).
- Watching a 20 min episode of a show as silly, joy filled, humorous and brilliant as The Simpsons allows your mind to exit one reality and enter another (in this case, the reality of yellow people who don’t age). The old me would have applied logic and sheer willpower to this scenario and immediately cast it down as a waste of time. But as I learn and grow older I realise that not every minute of life has to be filled with direct productivity and effectiveness. Its okay to let your mind wander, be bored, laugh and experience joy. One of the best things you can do before you sleep I’d argue is that. Which I’ve experienced to actuaklly help productivity in the long run alike to getting a good night sleep. Visual overwriting quiets the monkey mind, lightens your mood, has you feeling better and down-regulates your SNS (I don’t have evidence for this sorry I haven’t done a randomized controlled trial on watching The Simpsons before bed).
- For those freaking out about blue light, just do what I do: install a blue blocking program on your laptop – hook it up to your TV – put on some blue blocking glasses for extra safe measure and enjoy!
A-Typical Tips To Improve Sleep
- If you’re coming off a bad nights sleep resist the urge to sleep in – wake up at your normal time.
- Why? Your body has a 24h clock and it expects and thrives off regularity and if you change your wake up/falling asleep time you will confuse that 24h clock.
- If you sleep in you’re likely not to feel sleepy until later in the evening so you drift forward in time that time to fall asleep.
- If you’re in bed awake for 30min+ take a break and stop trying to fight sleep. The more we try to fight sleep the more stressed/anxious we become. and the further we push sleep awake from us. Read a book in red light until you feel sleepy again.
- Have a wind down sleep routine ritual. Many have this conception of sleep that it’s like a light-switch – for most sleep is like landing a plane, you have to give it time descend into good sleep.
- Remove/block all clock faces. If you’re struggling with sleep knowing what time it is in the middle of the night is not going to help your anxiety/stress about being awake.
If None Of This Works?
If you are still having trouble sleeping, you should be evaluated by your doctor for other problems that can interfere with sleep, including food sensitivities, thyroid problems, menopause, fibromyalgia, chronic fatigue syndrome, heavy metal toxicity, and, of course, stress and depression. Also, consider getting tested for a sleep disorder.
Alternative Treatment for Insomnia: Cognitive behavioral therapy for insomnia or CBTI.
- Just as effective as sleeping pills in the short term but and there are long term benefits to maintaining sleep improvements for 1-5 years.
- In cases of insomnia: Cortisol is down in evening but then right before bed it spikes again (sleep onset insomnia), sometimes spikes again in middle of night and keeping someone from falling back asleep (sleep maintenance insomnia)
- there is a non-pharmacological treatment but is just as effective as sleeping pills in the short-term. It is completely safe. And it is more efficacious in the long-term. And it’s called cognitive behavioral therapy for insomnia or CBTI.
- Based on its efficacious nature, and they’ve been done lots of randomized clinical control trials, it is just as powerful as sleeping pills in the short-term. But when you stop working with your therapist, and you work with a therapist for several sessions across several weeks, when you stop working with a therapist, you don’t go back to the bad sleep that you have. You continue on with your good sleep. Unlike sleeping pills, which is when you stop them, you have what we call rebound insomnia, which is that you tend to go back to the bad sleep that you are having, if not worse sleep that you are having before you started taking sleeping pills.Bright Light Exposure For Treatment of Bipolar & Depression Association
Other Treatment Options:
- Behavioral therapy is required: i.e. changes in mindset (meditation) and routine (less stressful activities close to bedtime such as work emails)
- Phosphatidylserine (400-600 mg): Peter uses this for jet lag circumstances (e.g., must go to bed when it’s only 2 pm in your brain) ⇒ “Phosphatidylserine really seems to move the needle, both in terms of your glucose response and your cortisol response.”
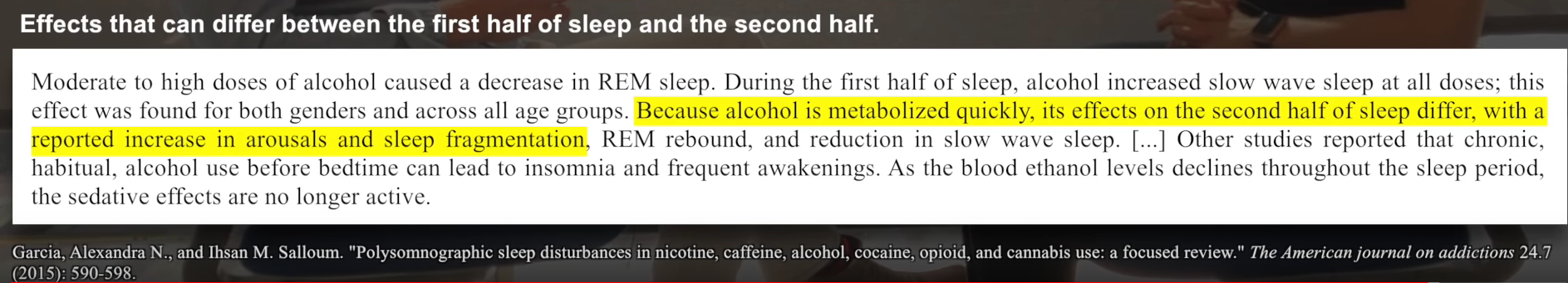
Morning Bright Light Exposure
What we do know is that getting 30 to 40 minutes of outside morning light is critical. Don’t put sunglasses on. Let that natural light penetrate your eye. There’s a retinal mechanism that goes through to your thalamus that then goes through the hypothalamus that regulates your circadian clock. You need that light penetration. You’re losing all of that good stuff if, or some of it, if you put shades on. – MW
Drawbacks to Sun Damage:
- Sun damages your DNA and can make you age faster and long toxic levels of sun exposure can contribute to benign or malignant melanomas.
Benefits:
- Nitric oxide benefits
- NO enhances blood flow, promotes blood vessel elasticity, lowers blood pressure, and functions as a signaling molecule in your brain and immune system
- Sun exposure helps to establish and set your circadian clock
- Bright light exposure has benefits in preventing myopia (shortsightedness)
How Much Sun Exposure Is Safe?Sensible exposure to UVB light (adequate exposure without allowing your skin to burn) may actually protect you from melanoma, whereas UVA radiation is associated with skin damage. For example, indoor workers actually have a higher risk of melanoma than outdoor workers, suggesting that chronic sun exposure may indeed have a protective effect. – Dr. Joseph Mercola
Sunscreen:Sunscreen unfortunately blocks Vit D synthesis which is why supplementing with Vit D is necessary for almost everyone who uses sunscreen.
Mineral Sunscreen: COOLA
- Ingredients in mineral sunscreens like zinc oxide and titanium dioxide — are “generally recognized as safe and effective.” by the FDA.
Chemical Sunscreen:
- We don’t yet know the effects of chemical sunscreens whose ingredients get absorbed into the bloodstream.
Why To Not Wear Sunglasses All The Time
- The retina in your eyes helps you to register how bright the light is that you’re being exposed to. And then, that causes a secretion of specific hormones that keep you safe from the sun, specifically, the sunlight. It will stimulate your pituitary glands via the optic nerve to produce a hormone that triggers melanocytes in your skin to produce more melanin. And, that allows you to tan and offer some protection from excess UV radiation. And, when you wear sunglasses, less sunlight reaches your optic nerve so less protective melanin is made and you have a higher risk of a sunburn and more carcinogenicity (tendency of a chemical to induce tumors) and a less attractive tan.
- As a matter of fact, one of the best things you can do for your skin and for protection from UV radiation, in addition, just not spending excess time in high amounts of UVA and UVB, is to avoid the use of sunglasses when you’re out in the sun.
- Also, to damage your eyes and create cataracts because without the UV light hitting your eye, the pupil and iris do not adjust properly to block the incident amount of light. So, it’ll let in a ton of the high-energy blue wavelengths because the UV stimulus has been blocked.
- But when you’re driving at night car headlamps are a notorious source of concentrated blue light from LED. So, if you have sunglasses, wear them at night if you don’t have blue blockers.
- Correlation data suggests that the eyes send a signal to your skin to produce more melanin, the pigment that causes you to tan, in response to brighter sunlight. If you wear sunglasses you hamper this process.
- So, another way to improve your body’s ability to make Vitamin D is to toss the shades. Don’t stare at the sun or anything, and if you go hiking in the snow or are outside for a long time on a bright day, feel free to use shades rather than squinting the whole time. I try to avoid using them but I’m no masochist. However, for a simple 20-minute session in the sun, you should be fine without them.
Skin Photoreceptors
- Even if you travel with the sleep mask, light-sensing photoreceptors that go far beyond the eyes are actually something that every human has. So, there are a number of different photoreceptors that we find on our skin. These are non-visual photoreceptors. And, what that means is that on your skin, your subcutaneous fat, your central nervous system, and a host of other areas in your body, including your blood vessels, you actually have light-activated photoreceptors that respond to wavelengths of light
- Melanopsin: A study at Johns Hopkins University relatively recently discovered something called melanopsin inside your blood vessels. And, melanopsin is one of the photoreceptors that’s used in non-visual photoreception. They found that this light-sensitive protein, this melanopsin, can regulate the contraction and relaxation of your blood vessels and can be damaged by exposure to artificial blue light. These melanopsin cells signal the circadian clock.
- Neuropsin: There’s another photoreceptor called neuropsin. And, that’s primarily found in the retina, but it’s also located on your skin. And, it’s a light-sensitive pigment that helps to regulate your body’s master circadian rhythm clock. And, that’s not only why going out in the sunshine during the day can be so beneficial for regulating your circadian rhythm, but it’s also why even if you’re wearing a sleep mask, even if you have blackout curtains or whatever in your room, if parts of your skin other than your eyes are exposed to light, it does affect your circadian rhythm.
Skin Cancer Is A Product of Toxic Sun Exposure/Lack Of Exposure from Modern Lifestyle
- When people went further north with less light, at least in Europe, there were mutations that were adapted so that we could assimilate more light and generate more vitamin D and get more of the benefits of the sun even with less light.
- So, for example, if someone lived out in the sun from winter to summer, the transition, the build-up that would occur of what we call the solar callus, which is the body’s natural sun protection mechanism, and it’s built out of keratinocyte cells that basically die upon exposure to sunlight and scatter their DNA, which is the ultimate absorber of UV light DNA is designed. So, that’s what these keratinocyte cells do, and they’re built up basically as the spring goes into summer each year from a winter to a summer.
- Now, the issue is that now we no longer have this natural build-up process. So, I would go as far to wager that sunburns were almost completely non-existent because if you live, for example, in Norway or Germany or England, as the sun came back slowly and you’re a wild ancient human wearing just a loincloth, which even Julius Caesar reported that’s pretty much all the Germans wore when he was facing them, it was their culture, even in the winter, and they would bathe in rivers and whatnot, cold rivers, surprise, surprise, for the health benefits. So, you would be getting that build-up, that solar callus such that by the time the strong summer sun came around, you’d be able to handle it. And the body contains these natural mechanisms where we know just exactly how much light we need to get.
- See, if we get too hot, we go in the shade. But now, today, we have this issue where we go into the sun. And because we’ve been living in entirely indoor lifestyle, the body is just begging, begging, begging for more and more and more sun, but the skin hasn’t adjusted. So, it isn’t that the sun and ultraviolet light causes skin cancer; it’s that man’s modern lifestyle and disconnection from sunlight has created an environment that allows us to obtain toxic, extremely high doses of ultraviolet light, which we would never have obtained previously in evolution leading to, for example, potential genetic mutation leading to things like skin cancer. But to blame it on the sun is not accurate. It’s a product of human life and modern human life.
- Outdoor Worker Effect: For example, some authors on the subject have written, it’s called the outdoor worker effect when a chronic tan naturally waxes and wanes with the sun, growing darker with the summer, then fading with winter light. In the ancient pattern of life, human appearance would track the seasons as it does for other animals like the bear and its winter coat. The modern indoor worker, especially in wealthier classes, grows pale inside offices, homes, and malls, and plunges into irregular bouts of excessive sunlight on beach vacations or long weekends. This sudden intense intermittent pattern of sun exposure heightens melanoma risk, says Bruce Armstrong, internationally known–he’s an internationally known Australian epidemiologist and former deputy director for the International Agency for Research on Cancer. And he was a co-author of this study in which they were making these conclusions.
- Study: a 1980 study by the London School of Hygiene and Tropical Medicine and the University of Sydney’s melanoma clinic found that the incidence of malignant melanomas was considerably higher in office workers and individuals who are regularly exposed to artificial light due to lifestyle or occupation. Those who had the lowest risk of developing skin cancer were those whose main outdoor activity was sunbathing. Twice the risk of developing melanoma was found in office workers who had to work indoors all day under fluorescent lights. Fluorescent office lights can cause mutation in cultures of animal cells. Dr. Shah, who is the main researcher on the study, concludes in both Australia and Great Britain, melanoma rates were high among professional and office workers and lower in people working outdoors. That’s very interesting.
- Practicality: Yes, excessive exposure to the sun unprepared can cause, for example, skin cancer. However, if one builds up a healthy solar callus on a regular basis, one can absolutely expose oneself to two to three hours of sunlight at the right times of day. But again, we have to listen to our body and feel its too hot get in the shade.
Contact Lenses:
- Contact lenses are also blocking UV light. Very not good. But also, they’re reducing oxygen levels reaching the cornea, which is the only tissue in the body that doesn’t receive oxygen from bloodstream. It’s designed to get it directly from the air. The cornea is very dense in mitochondria and it requires tremendous amounts of oxygen to function as a result.
Skin Photoreceptors
- Even if you travel with the sleep mask, light-sensing photoreceptors that go far beyond the eyes are actually something that every human has. So, there are a number of different photoreceptors that we find on our skin. These are non-visual photoreceptors. And, what that means is that on your skin, your subcutaneous fat, your central nervous system, and a host of other areas in your body, including your blood vessels, you actually have light-activated photoreceptors that respond to wavelengths of light
- Melanopsin: A study at Johns Hopkins University relatively recently discovered something called melanopsin inside your blood vessels. And, melanopsin is one of the photoreceptors that’s used in non-visual photoreception. They found that this light-sensitive protein, this melanopsin, can regulate the contraction and relaxation of your blood vessels and can be damaged by exposure to artificial blue light.
- Neuropsin: There’s another photoreceptor called neuropsin. And, that’s primarily found in the retina, but it’s also located on your skin. And, it’s a light-sensitive pigment that helps to regulate your body’s master circadian rhythm clock. And, that’s not only why going out in the sunshine during the day can be so beneficial for regulating your circadian rhythm, but it’s also why even if you’re wearing a sleep mask, even if you have blackout curtains or whatever in your room, if parts of your skin other than your eyes are exposed to light, it does affect your circadian rhythm.
Bright Light Exposure For Treatment of Bipolar & Depression Association
Exposing humans to 10,000 LUX 7 hours a day lowered their cortisol response during the rising phase in the morning when it’s usually the highest. (Acute effects of bright light exposure on cortisol levels – 2010)Even on a cloudy day you can be exposed to 5000 LUX which is a lot compared to sitting in your average room.
The Medical Industry Contradiction on Sleep
- Doctors on average have only 2~ hours of sleep education in the medical curriculum yet it’s 1/3rd of their patients life
- Sleep is a life support system, and it is mother nature’s best effort yet at immortality. And it’s a key to disease, and it’s a key to potentially helping treat or eou know, most doctors don’t ask how much sleep that you’re getting despite it being this fundamental, you know…Sleep is a life support system, and it is mother nature’s best effort yet at immortality. And it’s a key to disease, and it’s a key to potentially helping treat or even prevent disease. Most doctors don’t ask because most doctors aren’t educated.ven prevent disease. – MW
- Residents working a 30h shift are 460% more likely to make diagnostic errors in the ICU relative to when their working 16h.
- If you have elective surgery you should ask your surgeon how much sleep they had in the last 24h. If they’ve had 6 hours of sleep or less you have a 170% increased risk of major surgery error such as organ damage or hemorrhaging relative to that same surgeon being well rested.
- You wouldn’t accept surgical treatment at 3AM from a Doctor who was drunk. After 20h of being awake your as impaired as you would be if you were legally drunk. Yet Universities and medical institutions place young medical residents in positions of extreme decision making conditions while massively sleep deprived. Why do they do this? The history of it goes back William Halsted in the 1800s who set up the first resident surgical program in the US at Johsn Hopkins who was known for staying awake for days on end. How’d he manage that? Because he became an accidental cocaine addict as a result of studying the anesthetic properties of it. So he structured a program where he expected he’s residents to go toe to toe with him and that’s where this long drawn out practice of day long resident shifts come from. 1/5 medical residents will make a serious medical error due to insufficient sleep, 1/20 will kill a patient because of fatigue related error. If we could solve the sleep loss epidemic in medicine we could save more lives.
- Rebuttal: There are some concerns about contunity of care. If you keep switching residents out every 16h you wouldnt have continues patient care and that was a problem. But in France, Swedan and NZ they do not allow their residents to go over 14/16h shift and they train their residents in the same amount of time as other countries like the US doing longer shifts and if you look at the ranking of their medical health systems they rank far higher than the US. So you cant say longer work hours are necessary to create good docotors.
The medical profession: A culture that devalues sleep Walker looked at medical curricula of top 20 countries –
- most medical students get 1-2 hours of instruction about sleep during medical school
- This despite the fact that sleep takes up 1/3 of your life and makes such a huge difference to the 2/3 of life spent awake
Matthew’s article in The Lancet:Sleep Prescription for Medicine
- “I lay out the case for why both for patient and doctor, sleep is utterly essential, but profoundly absent.”
- If attending surgeon has slept only 6 hrs of previous 24, 170% greater chance of major surgical error
- If resident works 30 hour shift vs. 16 hour shift, 178% increased likelihood of car crash
- 1 in 5 residents make error due to insufficient sleep, 1 in 20 will kill a patient
- ER docs who work a 30 hr shift make 460% more diagnostic errors
- When lobby medical organizations and lay out this case, face incredible resistance ⇒ Minds made up, don’t want to hear facts
Patients
- The one place you need quality sleep to recover is the one place you get it least – which is a hospital ward.
- We could exit people out of hospital beds earlier, the data is already there for the neonatal (newborn) ICU – they used to leave bright lights on 24/7 which would prevent the signal for proper sleep cycle. If you regularize light in the neonatal ICU those infants have higher levels of O2 saturation because they were sleeping better, their weight gain was dramatically increased and they ended up exiting the neonatal ICU 5 weeks earlier. SIMPLE THINGS.\
- Solutions: 1. Sleep mask and eye plugs like an airplane. 2. Medical form that contains a box to fill out when you usually fall asleep and wake so staff can help facilitate your recovery via sleep.
My Simple 5 Step Airplane Sleep System
Let’s face it: from dry air to enormous doses of “dirty electricity”, to cabin pressure, circadian rhythm disruption, poor food and water and beyond, flying frequently on airplanes is about one of the worst things you can do for your sleep (and overall health). I get plenty of complaints from folks about how hard they find it to sleep on airplanes, but I personally sleep like a baby on just about every flight. How? Here’s my airplane sleep system:
- Request a window seat. It’s far easier to sleep when you can lean your head against the side of the airplane wall. Also, check out SeatGuru.com to learn more about the ideal seat on your flight.
- Use a J-hook travel pillow. These inflatable pillows are amazing, and the top-ranked travel pillow on Amazon. They work especially well for side sleepers in combination with the window seat trick but also work when you’re stuck in an aisle or center seat.
- Use earplugs combined with Sony or Bose noise blocking headphones
- Use a full wraparound sleep mask (Sleep Master Sleep Mask)
- Prior to putting on headphones, sleep mask and pillow, consume a few teaspoons of Reishi extract (I recommend the FourSigmatic blend), which allows you to sleep without waking up drowsy, combined with a good CBD source (20-40mg does the trick). [Source]
Sauna / Temperature Contrast Pre-Sleep
Sauna has been effective at aiding sleep – a great way to sleep is to create a high gradient of temperature, so the more negative the derivative of temperature the faster you’ll go to sleep and the longer you’ll sleep. So a sauna then cold shower then warm bed would theoretically help sleep greatly.
Exercise Shifting the Circadian Rhythm
Study: if you exercise at earlier in the day that advances the circadian rhythm to wake earlier. E.G. Working at 7:00 a.m or between 1 and 4 pm advanced the body clock to an earlier time. Meaning, if you want to start getting up earlier, exercise at 7:00 a.m., or if you want to delay your body clock to a later time, you want to start, say like sleeping in later or you’ve been waking up earlier than you want to, you wait to exercise until between 7:00 and 10:00 p.m. Context: when travel has thrown your circadian rhythm, shift work or you have thrown it off yourself.
Combating Jet Leg
- Dr. Satchin Panda for more info.
- Arriving During The Day: Upon arrivalget bright light exposure outside for 30 – 60min which initially starts the circadian clock and help reset the clock.
- Arriving In The Morning: Have a meal and start the circadian clock.
- Arriving In The Evening: Definitely fast and take melatonin.
Jet Lag Fix #2: Exercise
- Multiple studies have shown that exercise can regulate circadian rhythms. So as lousy and miserable as you may feel training after a long day of travel or a long few days of international travel, the sooner you can vigorously move after arriving at your final destination, the sooner you’ll bounce back from jet lag and normalize your circadian rhythm and sleep. But this doesn’t mean you have to do a killer WOD or an epic run when you get to your destination. My top three choices, if I’m feeling a bit blah after travel, are walking (barefoot if possible) in the sunshine or on a beach, swimming (preferably in relatively cool water, as you’ll learn about later), and, as mentioned in Fix #1, outdoor barefoot yoga. Finally, for each hour that I’m sedentary on an airplane, I do fifty air squats near the back of the plane or in any other open space I can find. Read more at:
Jet Lag Fix #4: Melatonin
- For travel across more than three time zones, I consume 60-80mg (yep, that’s a lot!) of melatonin prior to bed for rebooting my circadian rhythm upon arrival at my final destination. Melatonin is also a natural anti-inflammatory, which will help decrease inflammation that builds up during air travel. This is admittedly a huge amount of melatonin, so proceed at your own risk.
Jet Lag Fix #5:
- Water You’ve no doubt heard that you lose more water due to the dehydration that occurs while flying in the dry air at altitude—so you obviously need to drink more water to stay hydrated and beat jet lag. But I’ve been going beyond the normal recommendations and experimenting with very high water intake—and finding that it helps out quite a bit compared with the standard disappointingly tiny cup of water handed to me by the flight attendant every couple of hours. Instead, I’ve been drinking closer to 12–16 ounces of water (nearly a full bottle) each hour and feeling a distinct difference in sleep, mood, and energy upon landing. Just make sure to book an aisle seat or, if you’re in a window seat, make sure that your aisle-based airline partner is spry and willing to move every time you need to pee—or just politely ask to switch spots. Find water boring? Travel with a small bottle of organic stevia and add it to club soda or sparkling water to create a “cream soda esque” experience. Read more at:
Sleeping Pills (Ambien)
Sleeping pills we have on the market now (e.g. Ambien and Lunesta)
- 1) don’t produce naturalistic sleep
- 2) higher risk of death
- 3) higher risk of cancer
- Ambien isn’t part of that same class of drugs that alcohol is. It’s what we call a sedative hypnotic. It works on the same receptor, which is the GABA receptor. Now it tickles the GABA receptor in a different way to that which alcohol does. But what we found is that sleeping pills, they are sedating the brain. You’re not going into naturalistic sleep. If I look at the electrical signature of your sleep when you’re on a sleeping pill versus natural sleep, it’s not the same.
- Secondly, what we found is that those sleeping pills can often come with a grogginess in the morning and some forgetfulness.
Ambien-induced sleep resulted in a 50% unwiring of the connections that have been made during day rather than potentiating them.
we know that sleeping pills are associated with a markedly higher risk of death, as well as cancer, as well as your susceptibility to infection, particularly in pneumonia.
“As parents get more concerned about their kids who may have more anxiety, who are having sleep problems, they’re turning to pills . . . You’ve got a brain that is developing, a brain that need to wire itself up, strengthen connections, build and mature, it needs to learn, it needs to consolidate, and then you’re providing a form of sleep through medication that may actually be un-wiring that nervous system, and un-wiring those memories, rather than strengthening them. That frightens me, that frightens me a lot.”
Dreaming
Naps
History:
- Looking at hunter gatherers: Many sleep “biphasically” which means (long night sleep and then nap in afternoon)
- Hunter-gatherer tribes go to bed at 8:30- 9 pm
- Get 7-7.5 hrs of sleep
- Then nap in afternoon to make it about 9 hours total
- Gabra in northern Kenya
- San people in the Kalahari Desert
- It seems as though we are designed perhaps to be sleeping biphasically, which is a long bout at night, and then a siesta like nap in the afternoon
What is the efficacy of naps?
- Experiments show naps benefit learning, memory, immune function, & CV health and lower systolic BP
20 minute naps:
- “What we’ve found is that you can go down as low as about 20 minutes of a nap, and still see some mental benefits, in terms of things like learning and memory.”
90 minutes naps:
- “That gives the ability of the brain to go through the full 90 minutes cycle, so that the brain can go through all of the stages of non-REM sleep, stages one through four, and it gets the shot to get to REM sleep.”
In studies, nappers showed improvements in multiple parameters compared to controls who were relaxing in bed but not asleep
Should you nap if you have trouble sleeping at night?
- If hard to sleep at night, do not nap during day
- Adenosine builds up in body beginning when you get up
- The more builds up, the sleepier you feel
- After 16 hrs you should have no to fall and stay asleep
- During sleep, the brain will clear adenosine away, remove 16 hours of accumulated adenosine
- If you nap during day, especially in late afternoon, harder to fall asleep because nap removed some of the adenosine
- That said… if you can nap regularly and are still able to fall asleep at night, naps are fine
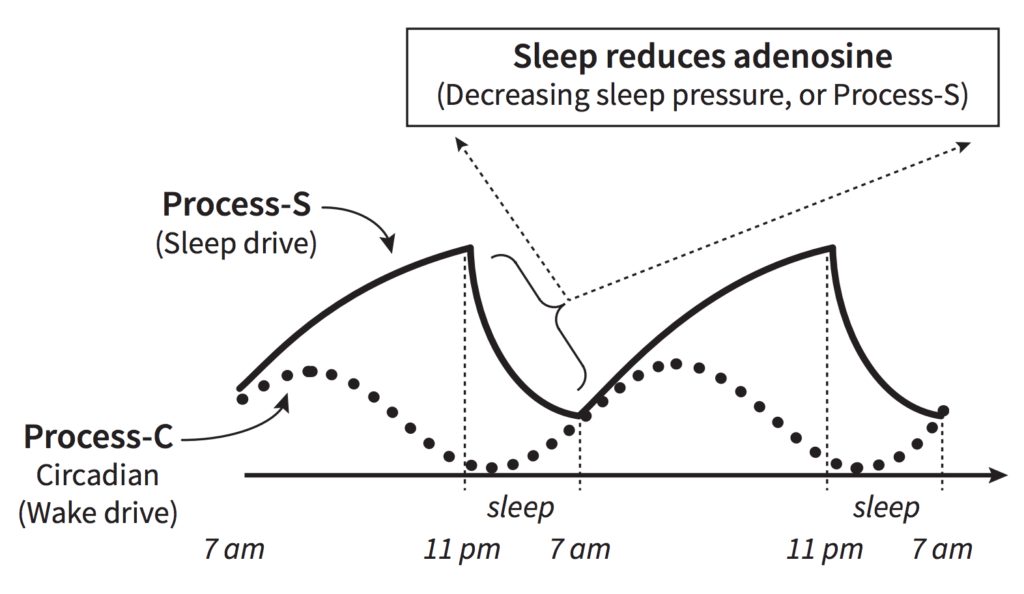
Combating Sleep Deprivation When It’s Inevitable.
Do you have any tips to improve sleep quality when I am bound to wake up every few hours during parenting babies?
- Naps: So, first of all, for improving sleep quality, when you’re waking up every two to three hours, I am a huge fan of micro-sleeps or micro-naps, and getting yourself into that micro-sleeping or micro-napping sleep phase as quickly as possible.
- Yoga Nidra: The other kind of like poor man’s version of this would be to go to YouTube and just grab any Yoga Nidra track. That’s Yoga Nidra. And Yoga Nidra is something that can also do a pretty decent job simulating a sleep cycle without you actually needing to fall asleep.
What to do when you wake up in the middle of the night and have to feed your baby or do something?Definitely keep a good pair of blue light blockers next to your bed stand. So, when you get up and you flip on the lights, you go in to see the baby, and maybe the baby monitor has a little bit of blue light flickering from it, or you’re checking your phone while you’re feeding the baby or whatever, you’re actually not downregulating melatonin and getting that big boost and wakefulness that you get from seeing blue light. So, I’m a fan of, right now, the company Ra Optics. They do really good red lens, blue light blocking glasses + red incandescent bulbs.https://raoptics.com/collections/glasses
Rotating Nights:I just think the idea of rotating nights with your wife versus rotating feedings allows you to go back and forth as far as getting a good solid night of sleep. I think that’s one thing to think about.
Exercise:during the day, research has shown that both short bursts of high-intensity exercise like 10 minutes of a kettlebell swing, or an air assault bike workout, or longer 40 to 60 minute bouts of easy aerobic endurance exercise are the two best forms of exercise to do if you’re in a sleep-deprived state. So, for your workouts, you can either do quick 10-minute high-intensity bursts rather than like go into the gym for a hard 60-minute session. Break that into six different short sessions during the day, or just do easy aerobic endurance exercise, or some variant of both. But those are the two flavors of exercise that work best and even seem to combat some amount of sleep deprivation.
Supplement: Qualia Nootropic (GREENFIELD2018 = 15% off)the two best supplements that I’ve found for combating sleep deprivation, one is any of the nootropics from the company Qualia, especially Qualia Mind or Qualia Focus. If you’re sleep-deprived, five capsules of Qualia Focus, or I think it’s seven to eight capsules of Qualia Mind for me. You can charge hard for like six to eight hours on that stuff. Have good word recall, good memory, good cognitive performance.
How To Wake Up Less At Night
- Avoid a big heavy meal close to bed especially with spices and high amounts of fat
- Complete physical activity 2-3h before bed.
- CBD, my restfulness goes through the roof with CBD. Now again, I take 600 to 100 milligrams. The three brands I kind of cycle through are I use the BioCBD sleep capsules which have some Ayurvedic herbs added to them like turmeric and ashwagandha and some other relaxing compounds, or I use Thorne soft gel hemp product, or for kind of the big guns, and I’ll link to all these in the shownotes, the Elemental Health maximum strength CBD, which is like a sublingual texture. If I do four dropperfuls of the elemental health stuff, I’m groggy the next morning, but only for like 20 minutes. Once I get up and around and get a cup of coffee in my system, I’m good to go
- Carbs before bed: If you are going to have a meal before bed, like if you are a dinner eater, save most your carbohydrates for dinner because you’ll get that serotonin release that actually enhances restfulness and that’s helped a lot with restfulness and with reducing sleep disturbances.
- Iris Program: From an artificial light standpoint, definitely install the Iris app. F.lux is okay, but Iris–F.lux will reduce some of the screen brightness, but Iris will affect screen temperature. You can change up your font type. You can switch to paper mode, or red light mode, or anything else. It’ll automatically adjust based on where your device happens to be in
- iPhone True Red Light Mode: And then on the phone, there’s a really great article, it’s on gadgethacks.com, about how to activate red light mode on your phone.
- Restfulness App: And then what I use is either SleepStream or something called Pzizz, P-Z-I-Z-Z. So, SleepStream, you can set that up for pink noise, which based on all the research of white noise, brown noise, all the different colors of noise,
- Lightblocking Sleep Mask: I found nothing that beats the Mindfold sleep mask. Again, that one was originally created for psychedelic journeying, but it blocks all light.
How Sleep Is Effected in a Caloric Deficit / High Stress
- During higher stress such as food scarcity your body releases higher amounts of catecholamines such as noradrenalin and cortisol. These hormones trigger glycogenolysis and lipogenisis to break down glycogen and FFAs.
- But norepinerphrin raises your sympathatic response to raise acute alertness/focus/mood which can interfere with sleep quality and make you more restless during the night or wake up earlier.
Playing a violent television game affects heart rate variability
- During violent (vs. nonviolent) gaming, there was significantly higher activity of the very low frequency component of the HRV and total power. During the night after playing, very low frequency, low frequency and high frequency components were significantly higher during the violent (vs. nonviolent) condition, just as total power. There were no significant differences between the three conditions (violent/nonviolent/no gaming) with respect to an index reflecting subjectively perceived sleep difficulties.
- Conclusion: Violent gaming induces different autonomic responses in boys compared to nonviolent gaming–during playing and during the following night–suggesting different emotional responses. Subjectively perceived sleep quality is not influenced after a single gaming experience. Future studies should address the development of the autonomic balance after gaming over longer time than a night, physiological adaptation to frequent gaming and potential gender differences.
What Type of Bed Should I Get?
Kelly Starrett:Soft is the solution for bedding’ . ‘Today’s modern human needs to sleep soft mattress. Ideally, you would be sleeping in a hammock. You Should be waking up in the morning feeling amazing without having to loosen up your back. Most athletes and people are extension-sensitive because of excessive sitting and extension-biased training(e.g., running, jumping/ squatting). Sleeping on a hard bed actually puts you into extension, which is the exact opposite of what you want if you’re extension-sensitive. Yes, you’d ideally be able to sleep on the floor and wake up feeling great, but We are not those people anymore due to excess sitting and inactivityKelly’s Mattress Checklist
- The softest mattress you can your hands on is ideal, but avoid those made solely of memory foam, as it locks you into extension.
- ‘Lie on a bed at a mattress store for 5 minutes. If you have o cross “our feet, your bed is too hard. [TF: Kelly found a Stearns and Foster model works well for him.]
- If you need to put a pillow under your legs to put you into flexion, then you need a softer bed.’ You should also focus on opening up hip extension.