Here’s an example of what usually happens to your testosterone in an aggressive long caloric deficit pushing <8% body fat.
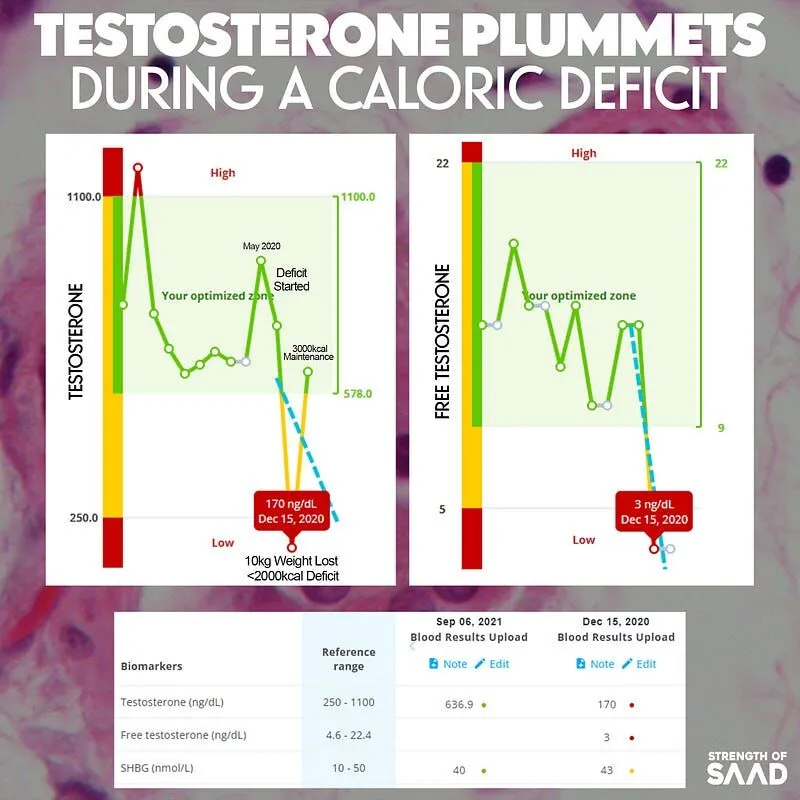
This is from a client who lost 10kg and got very lean (<40mm 9 site skinfolds and <8% body fat).
Lower T with very low body fat is one reason we see:
- Infertility (lower semen production + amenorrhea).
- Depression.
- Almost no libido.
- Sleep quality problems.
- Low energy, apathy and fatigue.
It is normal and expected to see testosterone plummet in response to a prolonged energy deficit with very low body fat levels. As you can see after 6 months of returning back to maintenance, gaining muscle and some fat, total and free T levels normalise.
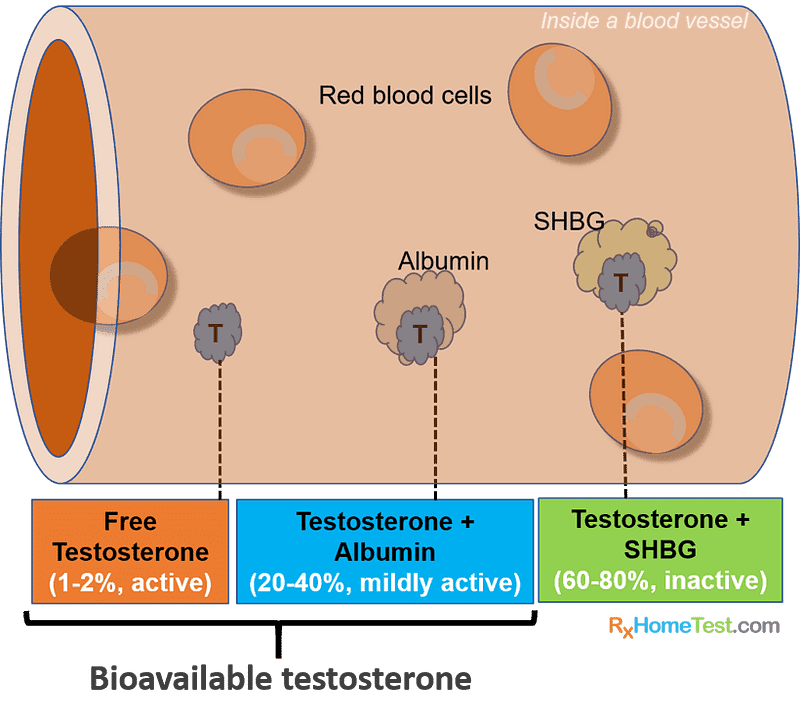
Testosterone, free testosterone and sex hormone-binding globulin (SHBG) are different forms of T in the bloodstream.
Bound Testosterone
T is bound to SHBG and albumin. These are proteins that bind and transport T through the body in a mostly inactive state (it can’t exert much, if any effect upon the body).
Unbound Testosterone
~1–3% of the T in the body is ‘free’ which refers to its unbound state not attached to any proteins. In this unbound state it is biologically active and can bind to receptors.
Free T is arguably the most important number, not total T, because free T is what’s bioavailable and what going to bind to the AR receptor to exert its androgenic effects of the synthesis of tissue, energy levels, libido etc.
Total testosterone on a blood test is the sum of all the testosterone in your blood (bound and unbound).
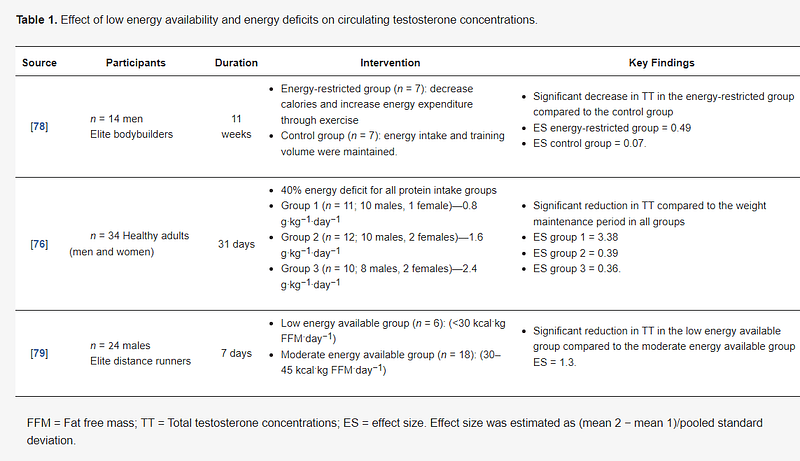
A 40% energy deficit (30% dietary restriction + 10% increase in physical activity above energy requirements) resulted in significant decreases in circulating T despite a high percentage of caloric intake being from protein.
Luteinizing Hormone
If you’re concerned about your T levels you also want to get your luteinizing hormone (LH) checked. LH is known for causing the ovaries to release an egg. So male’s don’t typically care about it and Doctors don’t typically look at it in males. But LH is the signal for the testes to make more T.
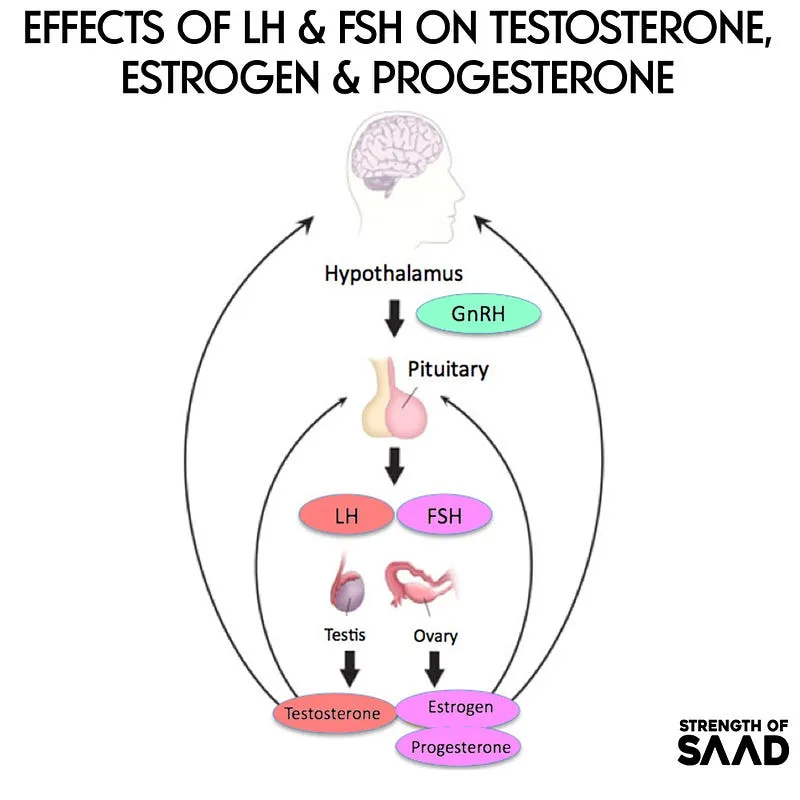
Caloric deficits have been shown to significantly reduce LH pulse frequency and amplitude during waking hours and increase at night in women. Another study showed LH pulsatility is harmed during an energy deficit in women.
Nutritional Co-Factors
Co-factors needed for testosterone metabolism include zinc and calcium to help bind SHBG.
A zinc ion is used on the conformation of the SHBG peptide chain and a calcium ion is needed to link what’s called a dimer (two identical molecules linked) together, keep it stable and improve steroid-binding activity.
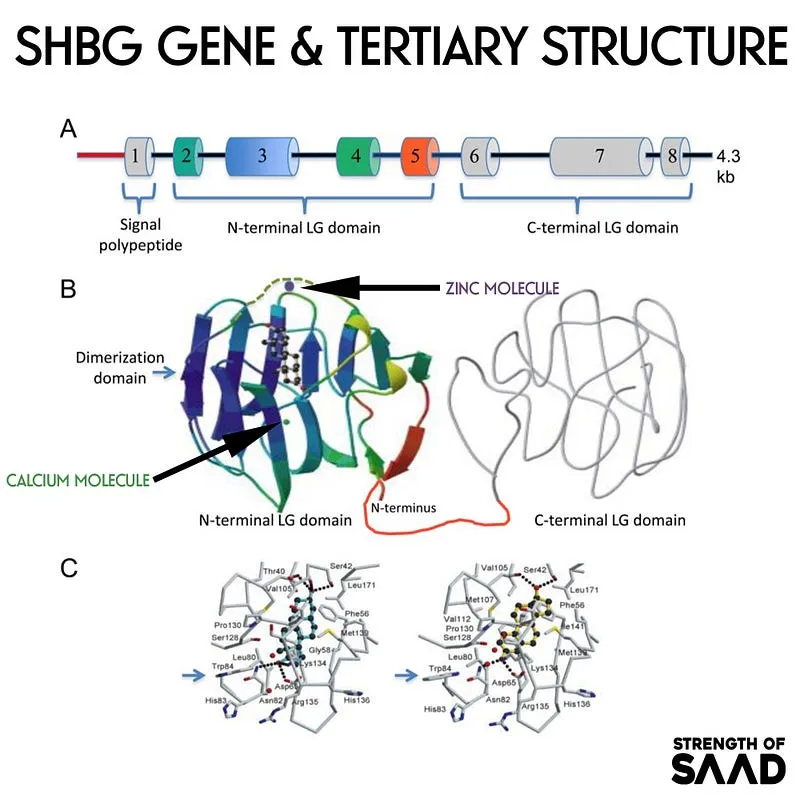
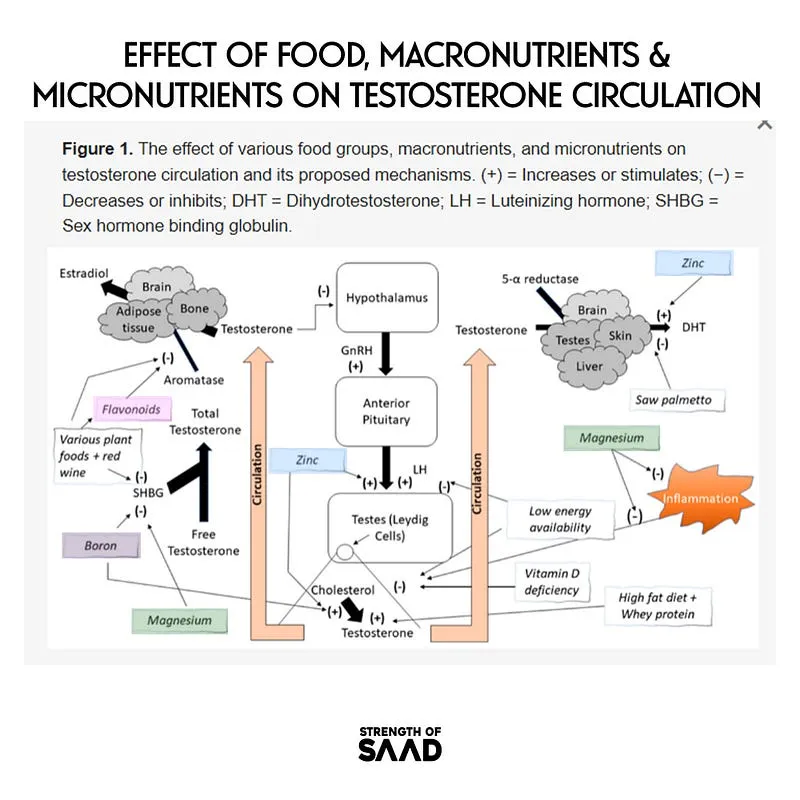
Often missing from the conversation of biochemistry is nutritional co-factors. So I wanted to highlight how deficiencies have the mechanistic probability to exert negative effects on testosterone. We now begin to see evidence of micronutrients like magnesium improving testosterone.
Final Thoughts & Practical Takeaway’s
- Manging nutritional deficiencies becomes paramount during an energy deficit.
- There is probably evidence that intaking optimal micronutrients (zinc, calcium, magnesium) before embarking on an energy deficit may improve one’s physiological response to the deficit.
- Low energy availability clearly has detrimental effects on physiology and the endocrine system. Though these effects are largely transient.